Triage, a critical process in healthcare, has multiple levels to classify the severity of emergencies. The most common systems use a three-tiered approach: Level 1 (immediate life-threatening), Level 2 (urgent but not life-threatening), and Level 3 (non-urgent). These levels guide medical professionals in prioritizing care, ensuring that those with the most critical needs receive immediate attention.
Understanding Triage: A Lifeline in Healthcare Emergencies
In the chaotic and often life-threatening world of healthcare emergencies, triage emerges as a crucial tool, a guiding light that sorts and prioritizes patients based on the severity of their injuries or illnesses. It’s a systematic process that ensures the most critical cases receive immediate attention, maximizing the chances of survival and recovery.
Definition and Role of Triage
Triage, derived from the French word meaning “to sort,” is the process of rapidly assessing and classifying patients into different levels of urgency. It serves as the foundation for prioritizing care, allocating resources, and directing patients to the most appropriate treatment areas. In emergencies, triage becomes the backbone of healthcare response, playing a pivotal role in saving lives and optimizing patient outcomes.
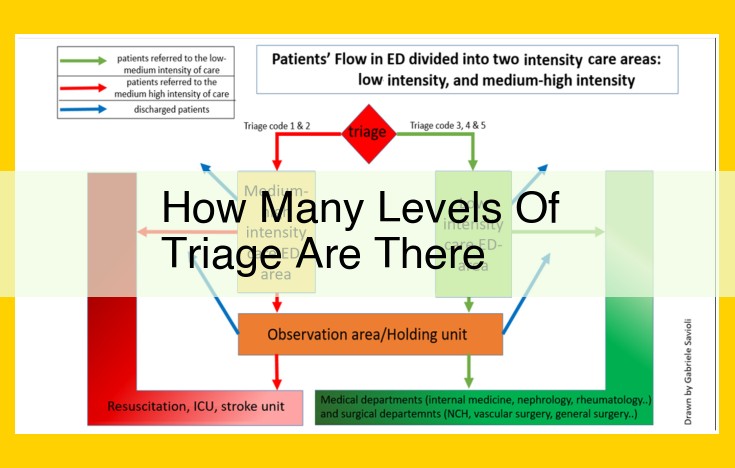
Levels of Triage: Classifying the Severity of Emergencies
In the realm of healthcare emergencies, triage stands as a crucial protocol that helps medical professionals prioritize patients based on the severity of their conditions. It ensures that those in dire need of immediate attention receive it promptly, while those with less critical injuries or illnesses are directed to appropriate care settings. Triage systems utilize color-coded tags or labels to categorize patients into different levels, each signifying the urgency of their medical needs.
-
Immediate Life-Threatening (Red Tag): These patients require immediate medical intervention. They may have severe injuries, such as life-threatening bleeding, cardiac arrest, or severe burns. Time is of the essence, and these patients are rushed to the emergency department for resuscitation and critical care.
-
Emergent (Orange Tag): Patients in this category have critical conditions that need urgent medical attention but are not immediately life-threatening. They may have fractures, serious infections, or severe asthma attacks. These patients are also prioritized for immediate care, but their conditions are not as critical as those in the red tag category.
-
Urgent (Yellow Tag): Patients with urgent conditions may have injuries or illnesses that require prompt medical attention within a few hours. They may have painful fractures, lacerations, or minor head injuries. These patients are typically seen by a doctor or nurse within a reasonable timeframe.
-
Semi-Urgent (Green Tag): Patients in this category have less severe conditions that require medical attention but are not urgent. They may have minor injuries, infections, or chronic conditions. These patients are usually seen by a healthcare provider within a few days.
-
Non-Urgent (Blue Tag): Patients with non-urgent conditions may not require immediate medical attention. They may have minor illnesses, such as colds or coughs, or non-acute pain. These patients are typically directed to self-care or follow-up appointments with their primary care physicians.
Understanding these triage levels is crucial for emergency responders and healthcare professionals. By accurately classifying patients based on the severity of their conditions, they can prioritize care, allocate resources, and ensure that those in most urgent need receive immediate medical intervention.
Entities Involved in Triage: A Symphony of Collaboration
Hospitals:
As the primary healthcare providers, hospitals play a crucial role in triage. Their emergency departments are equipped with trained personnel and specialized equipment to assess and prioritize patients’ conditions. Triage nurses, often certified in emergency nursing, conduct initial screenings, evaluating vital signs, symptoms, and medical histories to determine the severity of the emergency. Based on their assessments, they assign patients to appropriate treatment areas or refer them to other healthcare facilities.
Ambulance Services:
In pre-hospital settings, ambulance services serve as the first line of response to emergencies. Paramedics and Emergency Medical Technicians (EMTs), highly trained in triage protocols, assess patients on-scene. They provide immediate life-saving interventions and determine the most appropriate destination for medical care. Their triage assessments help streamline patient transfer to hospitals with the necessary resources and expertise.
Emergency Medical Professionals:
Firefighters and police officers, often the first to arrive at emergency scenes, also participate in triage. They provide initial assessment, securing the scene, and assisting with patient stabilization. Their knowledge of local resources and ability to coordinate with other emergency responders ensure that patients receive prompt and appropriate attention.
Centralized Triage Systems:
In large-scale emergencies or disasters, centralized triage systems are often established. These systems coordinate the efforts of multiple organizations, pooling resources and expertise to optimize patient care. Medical directors and incident commanders oversee the triage process, ensuring that patients are prioritized and resources are allocated efficiently.
Collaboration and Coordination:
Effective triage relies on seamless collaboration among all involved entities. Clear communication channels, standardized triage protocols, and shared patient information are essential to ensure smooth transitions between pre-hospital and hospital care. This collaborative approach optimizes patient outcomes by matching their needs with the appropriate medical facilities and interventions.
Concepts Related to Triage: Unraveling the Critical Factors
Triage, the art of prioritizing medical care in emergency situations, rests upon a foundation of critical concepts that guide the decision-making process. Understanding these concepts is paramount for ensuring the most effective and timely response to those in need.
Patient Acuity: Assessing the Severity
Patient acuity, the medical term for the urgency of a patient’s condition, lies at the heart of triage. Triage professionals use a variety of assessment tools to evaluate a patient’s vitals, symptoms, and overall presentation to determine the appropriate level of care required. By accurately assessing patient acuity, healthcare providers can prioritize the allocation of limited resources to those who need it most.
Priority Setting: Triage’s Guiding Principle
Priority setting, the systematic process of determining the order in which patients receive care, is the backbone of triage. Triage systems typically categorize patients into different levels of urgency, ranging from immediate life-threatening emergencies to non-urgent cases. Each level corresponds to a specific priority for treatment, ensuring that the most critical patients receive the immediate attention they require.
Disaster Medicine: Extending Triage’s Reach
Triage also plays a vital role in disaster medicine, where the influx of multiple patients with varying injuries and illnesses poses unique challenges. Triage protocols in disasters must be tailored to the specific circumstances, balancing the need for rapid assessment with the complexities of mass casualties. By effectively prioritizing patients during such events, healthcare professionals can maximize the number of lives saved and minimize long-term disabilities.
Key Takeaways
- Patient acuity: Determines the urgency of a patient’s condition, guiding resource allocation.
- Priority setting: Creates a systematic approach to prioritize patients based on their acuity, ensuring that the most critical cases receive immediate attention.
- Disaster medicine: Extends triage principles to manage mass casualties during emergencies, optimizing patient care outcomes.
Organizations and Policies Related to Triage: Setting Standards for Emergency Care
Triage, the systematic assessment and prioritization of patients in emergency situations, is a crucial aspect of healthcare. To ensure its effectiveness and consistency across various settings, government agencies, international organizations, and healthcare standards play a vital role in establishing triage protocols.
Government Agencies and Healthcare Standards
- National and Regional Health Agencies: Health ministries and other government agencies set guidelines and regulations for triage systems. They ensure that triage protocols are consistent with national healthcare priorities and adapt to regional needs.
- Healthcare Standards Bodies: Organizations like the American College of Surgeons and the European Resuscitation Council develop evidence-based standards for triage. These standards specify criteria for patient assessment, categorization, and management.
International Organizations
- World Health Organization (WHO): The WHO provides global guidance on triage systems. It develops tools and resources to support triage training and implementation in diverse healthcare settings.
- International Committee of the Red Cross (ICRC): The ICRC plays a role in establishing triage standards for humanitarian emergencies and armed conflicts.
Collaboration and Coordination
To ensure effective implementation and coordination, government agencies, international organizations, and healthcare standards bodies work together. They engage with healthcare professionals, researchers, and patient advocates to develop and refine triage protocols.
By establishing clear and evidence-based triage protocols, these organizations ensure that patients receive appropriate and timely care, even in high-stress emergency situations. These protocols improve patient outcomes, optimize resource allocation, and foster a culture of safety and efficiency in emergency healthcare systems.
Triage in Practice: Unraveling the Decision-Making Process
Triage is a crucial healthcare practice that determines the severity of medical conditions and prioritizes treatment based on patient acuity. Witness the riveting accounts of triage in action, where every second counts:
In the bustling Emergency Department, a frantic ambulance arrives, sirens blaring. Triage nurses swiftly assess the chief complaints and vital signs of multiple patients. One patient, clutching his chest, grimaces in agony. Immediate triage is assigned, as the nurses suspect an acute cardiac event.
Paramedics rush another patient in with a blunt head injury. Cervical spine immobilization and neurological assessment become paramount in this priority case. A third patient presents with severe abdominal pain and fever. Prompt triage reveals possible sepsis, warranting immediate antibiotic administration.
In a mass casualty scenario, triage plays an even more decisive role. Disaster responders categorize victims into four main triage categories: Red (immediate), Yellow (delayed), Green (minor), and Black (deceased). This rapid classification helps allocate limited resources effectively.
Triage teams rely on objective criteria to make critical decisions. Glasgow Coma Scale scores guide triage for head injuries, while chest pain severity and electrocardiogram (ECG) findings influence cardiac triage. Advanced medical equipment and telemedicine consultations further enhance the accuracy and timeliness of triage assessments.
Case Study: Saving Emily’s Life
Emily, a 50-year-old woman, collapsed at a shopping mall with sudden chest pain. Paramedics arrived within minutes and performed triage. Her ECG showed ST-segment elevation, indicative of an acute myocardial infarction (heart attack). Emily was classified as Red and rushed to the hospital for immediate cardiac catheterization. Emily’s prompt triage and subsequent treatment saved her life.
Best Practices for Effective Triage
In the fast-paced world of emergency healthcare, triage stands as a critical skill, enabling medical professionals to quickly and accurately assess the severity of patients’ conditions and prioritize their care. To ensure the most effective triage, adhering to best practices is paramount.
One fundamental best practice is utilizing standardized triage protocols. These guidelines provide a systematic approach for categorizing patients based on their presenting symptoms and vital signs. By following these protocols, healthcare providers can objectively and consistently determine the appropriate level of care for each patient.
Another key best practice is constant communication and collaboration. Effective triage requires seamless coordination among healthcare professionals, first responders, and patients. Clear communication ensures that all parties have a shared understanding of the patient’s condition and the recommended course of action.
Furthermore, ongoing training and education are essential for maintaining proficiency in triage skills. By staying up-to-date with the latest evidence-based practices, healthcare providers can improve their ability to accurately assess and prioritize patients, leading to better patient outcomes.
Additionally, utilizing technology can significantly enhance triage efficiency. Electronic health records (EHRs) can store and retrieve patient information, enabling a more comprehensive assessment. Automated triage systems can pre-screen patients, providing healthcare providers with valuable insights to inform their decisions.
Finally, regularly evaluating triage performance is crucial for improving the overall process. By collecting data on triage accuracy, timeliness, and patient outcomes, healthcare providers can identify areas for improvement and implement strategies to enhance triage efficacy.
In conclusion, adhering to best practices for effective triage is essential for optimal patient care. By utilizing standardized protocols, fostering communication, investing in training, embracing technology, and evaluating performance, healthcare providers can ensure that patients receive the right care, at the right time, and in the right place.
Ongoing Developments in Triage: Innovations and Future Directions
As the healthcare landscape evolves, so too does the critical role of triage. Advancements in technology, data analysis, and training are revolutionizing triage practices, paving the way for enhanced patient outcomes and streamlined emergency care.
Advancements in Triage Technology
Innovative triage tools are transforming the way healthcare professionals assess and prioritize patients. AI-powered algorithms, for instance, can analyze patient data in real-time and classify emergencies, ensuring that the most critical cases receive immediate attention. Mobile triage applications allow paramedics and emergency responders to conduct triage remotely, facilitating timely access to care in remote areas or during disasters.
Data Analysis for Improved Decision-Making
Big data is playing a crucial role in improving triage decision-making. By collecting and analyzing large datasets, healthcare providers can identify patterns and trends that inform triage protocols. Predictive analytics models can forecast patient acuity and predict outcomes, allowing for more accurate resource allocation and optimal patient care.
Enhanced Training for Triage Professionals
Simulation-based training is revolutionizing the education of triage professionals. Virtual reality (VR) and augmented reality (AR) technologies provide immersive environments where learners can practice triage scenarios and hone their critical thinking and decision-making skills. Continuing education programs ensure that triage professionals stay abreast of the latest advancements and best practices.
Future Directions in Triage
Ongoing research and development promise even more transformative innovations in triage. Wearable devices that monitor vital signs and symptoms could enable remote triage and early detection of emergencies. Artificial intelligence may play a role in triaging mental health emergencies, where traditional approaches can be challenging.
The future of triage is bright with the advent of cutting-edge technologies, data-driven decision-making, and enhanced training. These advancements will not only improve patient outcomes but also streamline emergency care and optimize resource utilization. As these innovations continue to emerge, the role of triage will remain indispensable in ensuring timely and appropriate care for all patients.