Periodontal disease development varies significantly based on individual susceptibility and contributing factors. Smoking, age, genetics, and oral hygiene play crucial roles. Poor oral hygiene allows plaque to accumulate, leading to gingivitis. If left untreated, gingivitis can progress to periodontitis, causing inflammation and destruction of gum tissue and underlying structures. The timeframe for this progression depends on the severity of contributing factors and can range from months to years.
Understanding Periodontal Disease: A Comprehensive Overview
- Definition and prevalence of periodontal disease
- Impact on oral and overall health
Understanding Periodontal Disease: A Comprehensive Overview
Periodontal disease, also known as gum disease, is a chronic inflammatory condition that affects the tissues surrounding your teeth. It’s a common problem, affecting nearly half of all adults in the United States.
The consequences of gum disease can extend far beyond your mouth. It has been linked to heart disease, stroke, diabetes, and other serious health conditions. That’s why it’s crucial to understand the causes, symptoms, and treatment options for periodontal disease.
The Causes of Periodontal Disease
The primary cause of periodontal disease is the buildup of plaque, a sticky film of bacteria that forms on your teeth. Plaque contains bacteria that feed on the sugars in your food and produce acids that attack your teeth and gums.
Over time, plaque can harden into tartar, which is more difficult to remove. Tartar can irritate your gums and cause them to become inflamed. This inflammation is the hallmark of periodontal disease.
Several factors can increase your risk of developing gum disease, including:
- Poor oral hygiene
- Smoking
- Diabetes
- Age
- Genetics
The Symptoms of Periodontal Disease
The early stages of gum disease are often painless. As the disease progresses, you may experience symptoms such as:
- Red, swollen, or bleeding gums
- Gums that are receding from your teeth
- Loose teeth
- Pain when chewing
- Bad breath
The Treatment of Periodontal Disease
The goal of periodontal disease treatment is to remove the plaque and tartar that is causing the inflammation. This can be done through a variety of methods, including:
- Oral hygiene: Brushing and flossing your teeth regularly is the best way to prevent and treat gum disease.
- Professional cleanings: Your dentist or hygienist can remove plaque and tartar from your teeth and below your gum line.
- Antibiotic therapy: Antibiotics may be prescribed to kill the bacteria that cause gum disease.
- Surgical interventions: In severe cases of gum disease, surgery may be necessary to remove infected tissue and restore the health of your gums.
Preventing Periodontal Disease
The best way to prevent gum disease is to practice good oral hygiene. Brush your teeth at least twice a day, floss daily, and see your dentist for regular checkups and cleanings.
If you have any of the symptoms of gum disease, see your dentist right away. Early diagnosis and treatment can help you prevent the progression of the disease and protect your oral and overall health.
Major Factors Contributing to Periodontal Disease: A Closer Look
Periodontal disease, also known as gum disease, is a common oral condition that can lead to tooth loss and other serious health problems. Understanding the factors that contribute to periodontal disease is crucial for preventing and effectively treating this condition.
1. Patient Factors
- Smoking: Smokers have a significantly higher risk of developing periodontal disease due to the harmful chemicals found in cigarettes that damage the gums and immune system.
- Age: As we age, our immune system naturally weakens, making us more susceptible to periodontal disease.
- Genetics: Some individuals are genetically predisposed to periodontal disease. Certain genes may increase the risk of developing a severe form of the disease.
- Timeframe: Periodontal disease is a chronic condition that develops over time. Prolonged exposure to risk factors can lead to a more severe and rapid progression of the disease.
2. Bacterial Factors
- Specific Oral Bacteria: Certain bacteria, such as Porphyromonas gingivalis and Aggregatibacter actinomycetemcomitans, are strongly associated with periodontal disease. These bacteria produce toxins that damage the gums and bone surrounding the teeth.
- Plaque Formation: Plaque is a sticky film of bacteria that accumulates on the teeth and gums. If not removed regularly, plaque can harden into tartar, which further irritates the gums and contributes to periodontal disease.
3. Immune Response
- Inflammatory Response: The body’s natural response to plaque buildup is inflammation. However, in some individuals, this inflammatory response becomes excessive and damages the gums and surrounding bone.
- Cytokine and Chemokine Production: The body releases cytokines and chemokines, which are small proteins that regulate the immune response. In periodontal disease, these proteins can overstimulate the immune system, leading to tissue destruction.
Understanding the interplay of these major factors is essential for gaining a comprehensive view of periodontal disease. By recognizing the connections between these contributing factors, we can develop more effective strategies for preventing, diagnosing, and treating this common oral health problem.
Specific Factors Influencing Periodontal Health
Maintaining optimal periodontal health hinges upon the intricate interplay of numerous factors. Among them, certain specific elements stand out for their profound impact on the delicate balance of our oral ecosystem:
Oral Hygiene:
- The cornerstone of periodontal health, impeccable oral hygiene practices (regular brushing and flossing) effectively remove plaque and bacteria, preventing their accumulation and mitigating the risk of gum inflammation and disease.
Specific Oral Bacteria:
- Specific oral bacteria, such as Porphyromonas gingivalis and Aggregatibacter actinomycetemcomitans, are notorious culprits in the pathogenesis of periodontal disease. They cleverly evade our immune defenses, unleashing enzymes that break down periodontal tissues.
Plaque Formation:
- Plaque, a sticky film of bacteria and food debris, is the primary culprit in plaque formation. When plaque accumulates on teeth, it harbors bacteria that secrete toxins, triggering an inflammatory response in the gums. Over time, this chronic inflammation can lead to irreversible damage to the supporting structures of teeth.
Inflammatory Response:
- The inflammatory response is the body’s natural defense mechanism against infection and injury. However, in the context of periodontal disease, a sustained inflammatory response can become a double-edged sword. While it initially aims to eliminate bacteria, prolonged inflammation can destroy healthy periodontal tissues.
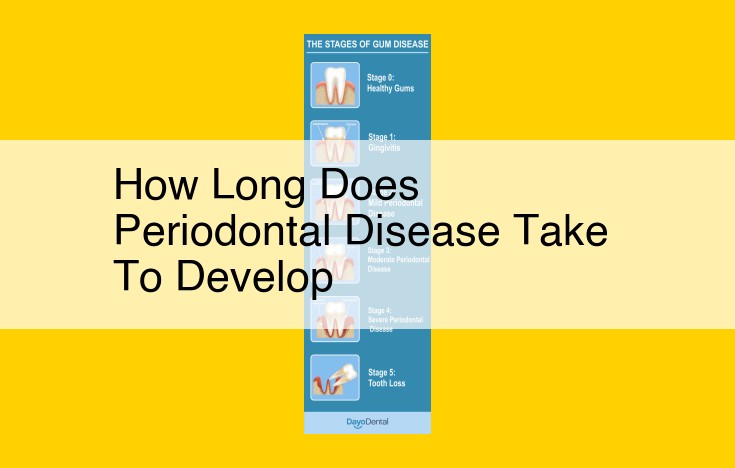
Gingivitis:
- Gingivitis is the first stage of periodontal disease, characterized by red, swollen, and bleeding gums. It occurs when the biofilm of bacteria and plaque irritates and inflames the gums, signaling the onset of periodontal destruction.
Periodontitis:
- Periodontitis is the advanced stage of periodontal disease, where the inflammatory response extends beyond the gums to affect the underlying bone and ligaments. As the condition progresses, it damages the supportive structures of the teeth, leading to tooth loss if left untreated.
Additional Contributing Factors to Periodontal Disease
Beyond the primary factors that directly influence periodontal health, several other aspects play a contributory role. These include:
-
Smoking: Nicotine and other chemicals in cigarettes impair the immune system, making individuals more susceptible to periodontal infections.
-
Age: As we grow older, our immune response generally diminishes, increasing the risk of developing periodontal disease. Reduced saliva production can also contribute to the problem.
-
Genetics: Certain genetic variations may predispose some individuals to periodontal disease by affecting their inflammatory response.
-
Cytokine and Chemokine Production: An overproduction of pro-inflammatory cytokines and chemokines can exacerbate periodontal inflammation.
-
Timeframe: The duration of periodontal infection is also a factor. Prolonged inflammation can lead to progressive tissue destruction.
These additional factors interact in complex ways to modulate the development and progression of periodontal disease. Understanding their interplay is crucial for developing comprehensive prevention and treatment strategies.
Understanding the Interplay of Factors
- How these factors interact and contribute to the development and progression of periodontal disease
Understanding the Interplay of Factors in Periodontal Disease
In the complex tapestry of periodontal disease, numerous factors play intricate roles, intertwining to drive its development and progression. Oral hygiene stands as a cornerstone, with plaque and bacteria forming a formidable alliance that instigates the disease process.
Poor oral hygiene allows plaque, a sticky film of bacteria, to accumulate on the teeth. Certain specific oral bacteria, such as Aggregatibacter actinomycetemcomitans and Porphyromonas gingivalis, are particularly adept at invading the gum tissues. These bacteria produce inflammatory mediators, setting off a chain reaction that damages the gums and supporting bone.
As the inflammation progresses, it triggers the release of cytokines and chemokines, which further escalate the battle within the gums. These chemical messengers recruit immune cells to the site, but their excessive presence can paradoxically exacerbate tissue destruction.
Smoking emerges as a potent accomplice, compromising the defenses of the gums and increasing their susceptibility to bacterial invasion. Age and genetics also hold sway, as older adults and individuals with certain genetic predispositions are more prone to periodontal disease.
The interplay of these factors drives a vicious cycle that leads to gingivitis, the milder form of gum disease. Left untreated, gingivitis can progress to periodontitis, a severe infection that destroys the gums and supporting bone, potentially leading to tooth loss and other systemic health complications.
By understanding the intricate web of factors involved in periodontal disease, we can develop comprehensive strategies to prevent its onset and mitigate its impact. Maintaining good oral hygiene, practicing regular dental check-ups, and addressing modifiable risk factors such as smoking can significantly improve periodontal health and overall well-being.
Consequences of Periodontal Disease: Unveiling the Hidden Dangers
Periodontal disease, a chronic infection of the gums and supporting structures, can have far-reaching consequences beyond your oral health. If left untreated, this insidious disease can silently inflict significant harm on your dental and overall well-being.
Dental Consequences
- Tooth loss: Advanced periodontal disease can destroy the jawbone that supports your teeth, leading to loose teeth and eventually tooth loss.
- Gum recession: The gums pull away from the teeth, exposing the sensitive roots and increasing the risk of tooth decay.
- Abscesses: Bacterial infection can form pockets in the gums, causing painful abscesses that can erode the bone and damage surrounding tissues.
Systemic Complications
- Cardiovascular disease: Studies have linked periodontal disease to an increased risk of heart attack and stroke. Bacteria from infected gums can enter the bloodstream and contribute to the formation of blood clots.
- Diabetes: Poor periodontal health has been associated with higher blood sugar levels in people with diabetes.
- Respiratory infections: Bacteria from periodontal disease can travel to the lungs, causing respiratory infections such as pneumonia.
- Pregnancy complications: Severe periodontal disease has been linked to premature birth and low birth weight in pregnant women.
It’s crucial to understand that periodontal disease often progresses silently, without causing any noticeable pain or discomfort. Regular dental checkups are essential for early detection and treatment to prevent these serious consequences.
Prevention and Treatment Strategies for Periodontal Disease
Periodontal disease is a common oral health issue that can lead to serious dental and systemic complications. The good news is that with proper prevention and treatment, you can effectively manage and prevent this condition.
Oral Hygiene
The foundation of periodontal disease prevention lies in maintaining good oral hygiene practices. This includes:
- Regular brushing: Use a soft-bristled toothbrush and fluoride toothpaste to brush your teeth at least twice a day.
- Flossing: Daily flossing helps remove plaque and bacteria from between your teeth and below the gum line.
- Tongue scraping: Use a tongue scraper to remove bacteria from your tongue, as it can contribute to periodontal disease.
Professional Cleanings
Regular dental checkups and cleanings are essential to maintaining periodontal health. A dental professional will:
- Remove plaque and tartar: These substances accumulate on your teeth and can irritate your gums.
- Check for signs of periodontal disease: Early detection and diagnosis are crucial for successful treatment.
- Provide oral hygiene instructions: Your dentist will guide you on proper brushing and flossing techniques.
Antibiotic Therapy
In some cases, antibiotic therapy may be prescribed to treat periodontal disease. Antibiotics can help eliminate bacterial infections and reduce inflammation.
Surgical Interventions
If non-surgical treatments have failed to control periodontal disease, your dentist may recommend surgical interventions. These procedures aim to:
- Remove diseased tissue: Diseased gum tissues and infected bone can be removed to promote healing and reduce infection.
- Correct bone defects: Bone defects caused by periodontal disease can be repaired and regenerated to improve gum support.
- Access deep pockets: Deep gum pockets can be surgically created to allow thorough cleaning and disinfection.
By implementing these prevention and treatment strategies, you can effectively manage periodontal disease and maintain optimal oral and systemic health. Remember, regular dental checkups, proper oral hygiene, and a healthy lifestyle are key to keeping your gums healthy and your smile bright.