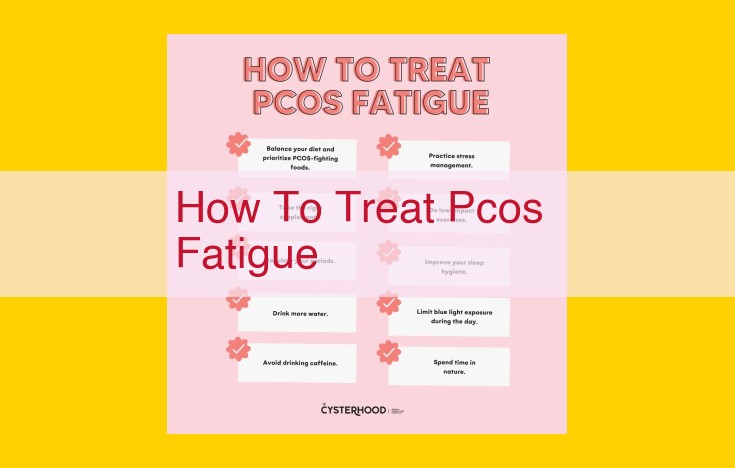
To combat PCOS fatigue, consider lifestyle modifications such as regular exercise, an anti-inflammatory diet, and stress management. Medications like metformin and birth control can regulate hormones and improve insulin sensitivity. Additionally, endocrinologists play a key role in diagnosing and treating PCOS through tests and procedures. Gynecologists assist with reproductive health concerns, addressing menstrual irregularities and pregnancy considerations.
Understanding Polycystic Ovary Syndrome (PCOS)
Embrace Comfort, Embrace Understanding: Exploring Polycystic Ovary Syndrome
Polycystic Ovary Syndrome (PCOS) is a prevalent hormonal disorder that affects millions of women worldwide. It is a complex condition that can manifest in a variety of ways, making it essential to understand its defining characteristics.
Defining PCOS and Its Prevalence
PCOS is characterized by an imbalance in the production of reproductive hormones, particularly androgen excess, which can disrupt normal functioning of the ovaries. This imbalance often leads to irregular periods, missed periods, or prolonged cycles. PCOS is also associated with the presence of polycystic ovaries, which contain numerous small follicles (cysts) instead of mature eggs.
Key Features of PCOS
The key features of PCOS include:
- Hormonal Imbalance: Elevated levels of androgens (male hormones), such as testosterone, can interfere with ovulation and cause excessive hair growth, acne, and male-pattern baldness.
- Insulin Resistance: Many women with PCOS have insulin resistance, a condition where the body’s cells do not respond well to insulin, the hormone that regulates blood sugar. Insulin resistance can contribute to weight gain and increased risk of type 2 diabetes.
- Chronic Inflammation: PCOS has been linked to chronic inflammation, which can affect various aspects of health, including metabolism, immune function, and fertility.
Lifestyle Modifications for PCOS Management: Empowering Women to Take Control
Polycystic ovary syndrome (PCOS) is a common hormonal disorder that affects women of reproductive age. While there is no cure for PCOS, lifestyle modifications can play a crucial role in managing its symptoms and improving overall health outcomes. Here are some key strategies to consider:
Exercise: Your Body’s Ally Against PCOS
Regular exercise is a powerful tool for combatting PCOS’s effects. Aim for at least 150 minutes of moderate-intensity exercise or 75 minutes of vigorous-intensity exercise per week. Physical activity helps:
- Reduce insulin resistance: Insulin resistance is a common feature of PCOS, and exercise improves the body’s ability to use insulin effectively.
- Lower inflammation: PCOS is associated with chronic inflammation, and exercise has anti-inflammatory effects.
- Improve body composition: Exercise helps reduce body fat and increase muscle mass, which can improve insulin sensitivity and hormone balance.
Diet: Nurturing Your Body from Within
Focus on a balanced diet rich in low-glycemic and anti-inflammatory foods. Low-glycemic foods release sugar slowly into the bloodstream, preventing insulin spikes that can worsen PCOS symptoms. Anti-inflammatory foods help reduce inflammation throughout the body.
- Choose whole grains, fruits, vegetables, and lean protein: These foods are rich in fiber, antioxidants, and nutrients that support overall health.
- Limit processed foods, sugary drinks, and unhealthy fats: These foods can contribute to insulin resistance, inflammation, and weight gain.
- Consider a Mediterranean-style diet: This diet emphasizes fruits, vegetables, whole grains, healthy fats, and lean protein, which has been shown to be beneficial for women with PCOS.
Stress Management: Finding Inner Peace
Stress can exacerbate PCOS symptoms. Implement stress-reducing techniques into your routine to promote relaxation and overall well-being.
- Practice mindfulness meditation: Meditation helps calm the mind and reduce stress levels.
- Engage in deep breathing exercises: Deep breathing can help slow down the heart rate and reduce tension.
- Seek support from loved ones: Talk to friends, family, or a therapist about your experiences with PCOS and seek emotional support.
Remember, lifestyle modifications are an ongoing journey, not a quick fix. Be patient and consistent with your efforts. With time and dedication, you can harness the power of lifestyle changes to improve your health and well-being with PCOS.
Medications for PCOS Treatment: A Guide for Managing Symptoms
Polycystic ovary syndrome (PCOS) is a common hormonal disorder that affects women of reproductive age. While lifestyle changes are crucial for PCOS management, medications can play a significant role in alleviating symptoms and improving overall well-being.
Overview of PCOS Medications
- Metformin: _This medication improves insulin sensitivity, reducing insulin resistance and blood sugar levels.
- Birth control pills: _These contain hormones that regulate menstrual cycles, control acne, and reduce androgen levels.
- Anti-anxiety medications: _These medications can help manage the stress and anxiety associated with PCOS.
- Antidepressants: _They can alleviate mood swings and improve overall mental health.
The Role of Metformin
Metformin is a first-line medication for women with PCOS who have insulin resistance. It works by sensitizing cells to insulin, allowing them to absorb more glucose from the bloodstream. This reduces blood sugar levels, improves insulin sensitivity, and regulates menstrual cycles. Metformin can also reduce acne and body weight.
Birth Control Pills for PCOS
Birth control pills contain estrogen and progesterone. These hormones regulate menstrual cycles, reducing irregular bleeding. They can also suppress androgen production, alleviating symptoms such as acne, facial hair, and male-pattern baldness.
Medications for Mental Health
Stress and anxiety are common in women with PCOS. Anti-anxiety medications, such as clonazepam and buspirone, can help manage these symptoms. Antidepressants, such as fluoxetine and sertraline, can improve mood swings and enhance overall mental well-being.
Medications can provide effective relief from the symptoms of PCOS. By working closely with your healthcare provider, you can determine the best medication or combination of medications to manage your individual symptoms and improve your overall health. Remember, while medications play an important role, embracing a healthy lifestyle that includes regular exercise, a balanced diet, and stress management is essential for long-term PCOS management.
Endocrinology and PCOS: Unraveling the Hormonal Mysteries
Endocrinologists hold a crucial role in the diagnosis and management of Polycystic Ovary Syndrome (PCOS). These healthcare professionals specialize in the study of hormones and endocrine glands, making them experts in deciphering the hormonal imbalance that characterizes PCOS.
When seeking medical guidance for PCOS, endocrinologists will conduct a thorough examination, assessing your medical history, lifestyle factors, and symptoms. To confirm the diagnosis, they may order specific tests, including:
- Blood tests: These tests measure hormone levels, such as testosterone and luteinizing hormone (LH), to detect the hormonal imbalances associated with PCOS.
- Pelvic ultrasound: This imaging technique helps visualize the ovaries and identify the presence of cysts, a hallmark of PCOS.
Endocrinologists may also employ specialized procedures, such as:
- Glucose tolerance test: This test evaluates insulin resistance, a common feature of PCOS.
- Thyroid function tests: Thyroid problems can mimic PCOS symptoms, making it essential to rule out any underlying thyroid issues.
By interpreting these test results and considering your individual circumstances, endocrinologists can develop a tailored treatment plan to regulate your hormones and manage your symptoms. They may prescribe medications, such as:
- Metformin: This drug improves insulin sensitivity and may help regulate menstrual cycles.
- Birth control pills: These pills contain hormones that suppress ovulation and reduce androgen levels.
- Anti-androgen medications: These drugs block the effects of male hormones, which can contribute to PCOS symptoms.
In addition to medications, endocrinologists may recommend lifestyle modifications to support PCOS management, such as:
- Weight loss: Even modest weight loss can help improve insulin sensitivity and reduce PCOS symptoms.
- Regular exercise: Aim for at least 30 minutes of moderate-intensity exercise most days of the week.
- Healthy diet: Focus on whole, unprocessed foods that are low in glycemic index.
- Stress management: Techniques like yoga, meditation, or deep breathing can help reduce stress levels and improve PCOS symptoms.
By working closely with endocrinologists, women with PCOS can gain a comprehensive understanding of their condition and receive personalized treatment to manage their symptoms effectively and improve their overall well-being.
Gynecology and Polycystic Ovary Syndrome (PCOS)
Gynecologists: Essential Partners in PCOS Healthcare
In the intricate world of PCOS management, gynecologists play a pivotal role in ensuring the well-being of women affected by this complex condition. Their expertise extends beyond general medical care, encompassing a deep understanding of female reproductive health and its unique challenges in the context of PCOS.
Menstrual Irregularities: A Common Symptom, A Critical Concern
For many women with PCOS, irregular menstrual cycles are a hallmark symptom. These irregularities can range from infrequent periods to prolonged absence of menstruation. Understanding the underlying causes and managing these fluctuations is crucial for optimal health. Gynecologists provide guidance on lifestyle adjustments, hormonal therapies, and other interventions to regulate menstrual cycles and improve fertility.
Reproductive Health: Addressing Unique Challenges
PCOS can impact reproductive health in several ways. Women with PCOS may experience difficulty conceiving, increased risk of miscarriage, and potential complications during pregnancy. Gynecologists work closely with patients to assess fertility, provide support during pregnancy, and monitor for potential complications. Through specialized knowledge and personalized care, they strive to optimize reproductive outcomes for women with PCOS.
Pregnancy and PCOS: A Journey Requiring Specialized Care
Women with PCOS who become pregnant require close monitoring and specialized care. Gynecologists assess potential risks, such as gestational diabetes and preeclampsia, and provide ongoing support throughout pregnancy. They work with patients to manage symptoms, adjust medications, and ensure the health of both mother and baby.
By partnering with gynecologists, women with PCOS gain access to comprehensive and compassionate care that addresses their unique needs. From managing menstrual irregularities and reproductive challenges to navigating pregnancy, gynecologists empower women with PCOS to achieve their health and fertility goals.