To avoid observation status, understand its key players and the Medicare statute defining it. Ensure proper documentation and communication between physicians, patients, and hospitals. Consider the patient’s medical condition, estimated length of stay, and need for further diagnostic tests. Consult CMS guidelines and seek legal assistance if needed.
Entities Central to Observation Status
In the realm of healthcare, the concept of observation status plays a pivotal role in determining the course of treatment and financial implications for patients. This intricate landscape involves a network of key players, each with unique roles and responsibilities. Let’s delve into the entities central to observation status and their significance in this complex healthcare dynamic.
Patients: The Heart of the Matter
Patients are the primary beneficiaries or subjects of observation status. Their medical condition, symptoms, and overall health status determine whether they qualify for this temporary designation. Observation status allows for a period of close monitoring and assessment, typically for up to 48 hours, before a decision is made on whether to admit the patient to the hospital or discharge them home.
Physicians: Gatekeepers of Observation Status
Physicians hold the responsibility of assessing patients and determining whether observation status is appropriate. They gather relevant information through physical examinations, diagnostic tests, and patient history, carefully weighing the evidence to make informed decisions. Physicians play a crucial role in ensuring that patients receive the most suitable level of care, balancing the need for further monitoring with the potential risks associated with hospitalization.
Hospitals: Providing a Temporary Haven
Hospitals serve as the physical setting where observation status is implemented. They provide the necessary facilities and resources for patient monitoring, including observation units or dedicated observation beds. Hospitals work closely with physicians to ensure that patients receive appropriate care during their observation period, facilitating timely decision-making regarding their future treatment path.
Diving into Medical Terms: Understanding Observation Status
When navigating the complex healthcare system, encountering unfamiliar terms can be overwhelming. Observation status is one such concept that often sparks confusion. To shed light on this topic, let’s unravel its definition and delve into related concepts like inpatient admission and medical necessity.
Observation status refers to a specific category in hospitals where patients receive medical attention, typically for short-term stays (less than 24 hours). Patients under observation are not formally admitted as inpatients, but they undergo medical evaluations, monitoring, and treatments to determine the appropriate care plan.
In contrast, inpatient admission signifies a patient’s formal admission to the hospital for extended medical care. Inpatients receive ongoing treatment and supervision under the direct supervision of physicians throughout their stay.
Medical necessity plays a crucial role in determining whether a patient meets the criteria for observation status or inpatient admission. Medical necessity refers to the essential and appropriate healthcare services that are deemed necessary to diagnose or treat a patient’s condition.
Understanding these fundamental terms is essential for patients and healthcare providers alike. It helps in navigating the healthcare system effectively, ensuring patients receive the appropriate level of care, and fostering clear communication between all parties involved.
Regulatory Framework: Defining and Enforcing Observation Status Regulations
In the realm of healthcare, observation status holds a pivotal position, governing the classification and management of patients who require medical attention but are not deemed eligible for inpatient admission. Understanding the regulatory framework that governs observation status is crucial for patients, providers, and healthcare institutions alike.
At the heart of this framework lies the Medicare Observation Status Statute, enacted in 1983. This statute empowers the Centers for Medicare & Medicaid Services (CMS) with the responsibility of establishing and enforcing regulations that define and delineate the criteria for observation status.
CMS plays a multifaceted role in this domain. It issues guidelines and interpretive memoranda to provide clarity and guidance on the application of observation status regulations. These guidelines specify the criteria that must be met for a patient to be classified as an outpatient with observation status, as opposed to an inpatient requiring hospitalization.
CMS also conducts audits and reviews to ensure compliance with observation status regulations. These reviews scrutinize medical records and documentation to verify that patients are appropriately classified and that their care is consistent with the established criteria.
Noncompliance with observation status regulations can have significant consequences. Hospitals may face financial penalties and reimbursement denials if they improperly classify patients as outpatients with observation status when they should have been admitted as inpatients. Patients, on the other hand, may experience financial hardships if they are responsible for paying for services that should have been covered by Medicare as an inpatient.
To ensure fairness and impartiality, CMS has established an Independent Dispute Resolution Entity (IDRE). This entity adjudicates disputes arising from observation status determinations. Patients and providers can appeal observation status decisions to the IDRE, which conducts an independent review of the case and issues a binding decision.
Patient Perspectives: Navigating the Maze of Observation Status
When navigating the intricate healthcare system, patients often encounter the concept of observation status. This designation, which often lingers between inpatient and outpatient care, can have a significant impact on their financial implications and access to care.
For patients, observation status can translate into higher out-of-pocket costs. Inpatient admissions typically qualify for coverage under major medical insurance plans, while observation stays may fall into a coverage gray area. As a result, patients may be responsible for a larger portion of the bill, including deductibles, copayments, and coinsurance.
Another concern arises when observation status limits access to certain benefits. Patients in observation may not qualify for skilled nursing facility coverage, which can be crucial for those requiring ongoing medical care after discharge. Additionally, some prescription drug plans may not cover medications administered during observation stays.
To mitigate these challenges, patients should proactively communicate with their insurance providers to clarify their coverage options under observation status. They can also seek support from patient advocates or hospital financial counselors to ensure they fully understand the financial implications and access limitations associated with this designation.
Understanding the nuances of observation status empowers patients to make informed decisions about their care. By being aware of the potential financial and access considerations, they can proactively advocate for their rights and ensure they receive the necessary medical attention without facing unnecessary financial burdens.
Provider Considerations in Observation Status Management
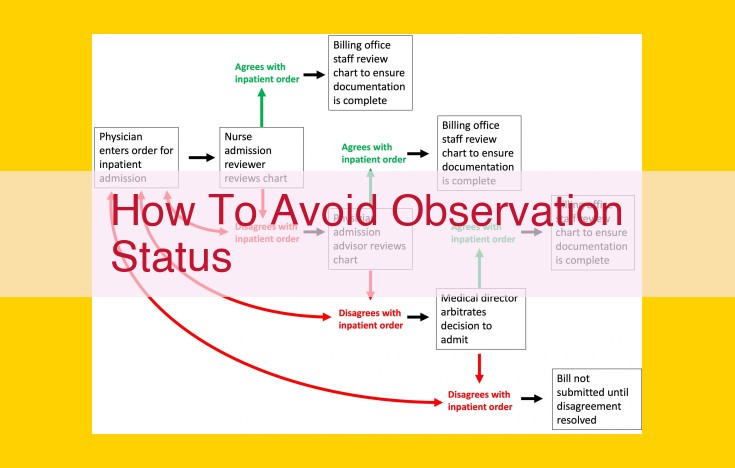
Determining and managing observation status poses significant challenges for physicians and hospitals due to its complex regulatory framework. A key challenge lies in accurately assessing the medical necessity of admitting a patient as an inpatient versus observation status. Physicians must carefully review patient records and consider factors such as the severity of symptoms, potential risks, and need for immediate medical intervention.
Another complexity arises from the varying interpretations of observation status regulations among hospitals and providers. This inconsistency can lead to disparities in patient care and confusion for both patients and medical professionals. Ensuring compliance with Medicare guidelines requires hospitals to establish clear policies and procedures, which can be time-consuming and resource-intensive.
Furthermore, providers must navigate the complexities of the appeals process for disputed observation status decisions. If a patient or provider believes that an observation status placement is inappropriate, they can initiate an appeal with the hospital or the Centers for Medicare & Medicaid Services (CMS). This process can be lengthy and requires thorough documentation and evidence to support the appeal.
Understanding the financial implications of observation status is crucial for both patients and providers. Hospitals may be penalized for inappropriately admitting patients as inpatients, while patients may face unexpected costs if their observation stay exceeds a certain number of days. Providers must effectively communicate these implications to patients to ensure informed consent.
In addition to these challenges, providers must stay abreast of current trends and policy changes in observation status management. CMS regularly updates guidelines and regulations, requiring providers to adapt and adjust their practices accordingly. It is essential to engage in continuing education and stay informed through industry publications and webinars to remain compliant.
By acknowledging and addressing these challenges, providers can improve their management of observation status. This involves establishing clear criteria for patient placement, adhering to Medicare guidelines, and navigating the appeals process effectively. Through collaboration and effective communication, providers can ensure appropriate patient care, avoid financial penalties, and uphold the integrity of the observation status system.
Dispute Resolution: Navigating Observation Status Disputes
When disputes arise regarding observation status, a structured process is in place to resolve them fairly and efficiently. This process involves two primary avenues: appeals and the Independent Dispute Resolution Entity (IDRE).
Appeals Process
The first step in disputing an observation status determination is to file an appeal with the Medicare Administrative Contractor (MAC) responsible for processing claims in your area. The appeal should provide evidence and rationale supporting the request for a change in status. The MAC will review the appeal and make a decision within a predetermined timeframe.
If dissatisfied with the MAC’s decision, you may request a reconsideration or appeal to the Quality Improvement Organization (QIO) assigned to your state. The QIO will conduct an independent review and issue its own decision.
Independent Dispute Resolution Entity (IDRE)
In cases where the QIO’s decision is also unsatisfactory, you may seek further review through the IDRE. The IDRE is an independent organization that conducts impartial reviews of observation status disputes.
The IDRE’s review process involves a two-tiered approach. First, a preliminary review is conducted to determine if the case meets the criteria for a full review. If the criteria are met, the case is assigned to an independent reviewer, who will conduct a thorough analysis and issue a decision.
The decision of the IDRE is binding on all parties involved in the dispute. It provides a final and impartial resolution to observation status disagreements, ensuring fair treatment for both patients and healthcare providers.
Current Trends and Future Implications of Observation Status
The landscape of observation status is constantly evolving, with recent developments and emerging trends shaping its future trajectory. Here’s an overview of the most significant changes affecting this complex healthcare landscape:
Policy Shifts and Regulatory Updates
Policy Changes
CMS has consistently revised its regulations on observation status, aiming to clarify guidelines and address ongoing challenges. These changes aim to streamline processes, reduce disparities, and enhance the quality of care for patients.
Regulatory Updates
The Independent Dispute Resolution Entity (IDRE) has undergone significant updates, empowering patients and providers with an impartial and efficient avenue to resolve observation status disputes. These refinements ensure that grievances are addressed promptly and fairly.
Technological Advancements
Telemedicine and Remote Monitoring
Technological advancements have revolutionized healthcare delivery, extending beyond traditional hospital settings. Telemedicine platforms and remote monitoring devices enable patients to receive care in the comfort of their homes, potentially reducing the need for observation status admissions.
Artificial Intelligence (AI)
AI algorithms are being explored to analyze patient data and predict the likelihood of hospitalization. This technology has the potential to enhance the accuracy of observation status decisions, freeing up healthcare professionals for more critical tasks.
Emerging Trends
Focus on Value-Based Care
The healthcare industry is shifting towards value-based care, where reimbursement is tied to patient outcomes rather than the number of procedures performed. This paradigm shift encourages providers to make more judicious decisions about observation status utilization, ensuring appropriate care for patients while optimizing healthcare resources.
Emphasis on Patient-Centered Care
Patients are becoming increasingly involved in their healthcare decisions, and this trend extends to observation status. Shared decision-making empowers patients to understand their options and actively participate in the decision-making process, promoting transparency and fostering trust between patients and providers.