I. Medical Terms
- Blood clot: coagulo sanguíneo
- Thrombus: trombo
- Embolus: émbolo
- Coagulated blood: sangre coagulada
Understanding Blood Clots: Types and Mechanisms
In the realm of human health, the intricate network of blood vessels plays a vital role in delivering life-sustaining oxygen and nutrients to every cell in our body. However, within this delicate system, a potentially dangerous phenomenon lurks: blood clots.
Blood clots, also known medically as thrombi or emboli, form when blood becomes abnormally sticky and clumps together. Thrombi, or stationary clots, are typically found in blood vessels, obstructing blood flow. In contrast, emboli, or floating clots, break free from their original location and travel through the bloodstream, potentially causing severe complications downstream.
Notably, coagulated blood is not the same as a blood clot. Coagulation, or blood clotting, is a crucial defense mechanism that prevents excessive bleeding when injured. However, when this process goes awry, it can lead to the formation of harmful clots.
By understanding the different types of blood clots and their mechanisms, we can better prevent and treat these potentially life-threatening conditions.
The Vascular System and Blood Clot Formation
The intricate network of arteries, veins, and blood vessels plays a crucial role in both preventing and promoting blood clots. Understanding their functions is essential for comprehending the dynamics of clot formation and its potential consequences.
Arteries, the oxygen-rich conduits that branch from the heart, are lined with a smooth endothelial layer that serves as a nonstick surface, resisting clot formation. However, when these blood vessels become inflamed or damaged, the endothelial lining can become compromised, creating an environment conducive to thrombosis (the formation of a blood clot within a blood vessel).
Veins, on the other hand, are responsible for returning deoxygenated blood back to the heart. Unlike arteries, veins have thinner walls and contain valves that prevent blood from flowing backward. However, these valves can become weak or damaged, especially with age, leading to a condition called venous insufficiency. This can cause blood to pool in the veins, increasing the risk of blood clot formation, known as deep vein thrombosis (DVT).
Blood vessels, both arteries and veins, are vital in regulating blood flow and maintaining proper blood pressure. When blood flow is slow or irregular, such as during prolonged sitting or inactivity, the risk of thrombus (a stationary clot) increases. Conversely, exercise and regular physical activity promote blood circulation, reducing the likelihood of blood clot formation.
Understanding the delicate balance between blood vessels and blood clotting is paramount for maintaining vascular health. By adopting a healthy lifestyle, including regular exercise, managing weight, and quitting smoking, individuals can significantly reduce their risk of blood clots and their associated complications.
Vital Organs: The Battleground of Blood Clots
When blood clots form in the arteries or veins supplying vital organs, they can unleash a devastating cascade of consequences. These clots, like tiny barricades, obstruct the life-giving stream of oxygen and nutrients, threatening the very function of these critical organs.
The Brain: A blood clot in the brain can lead to a stroke, a medical emergency that can manifest in various forms. From sudden weakness or numbness on one side of the body to speech difficulties and confusion, a stroke can leave lasting disabilities or even prove fatal.
The Heart: Clots in the heart’s arteries can lead to a heart attack, a life-threatening condition in which an area of heart muscle is starved of oxygen. Chest pain, shortness of breath, and arm or jaw discomfort are telltale signs of a heart attack, requiring immediate medical attention.
The Lungs: Blood clots in the lungs can cause a pulmonary embolism, a potentially fatal condition in which a large clot blocks the main artery in the lungs. Symptoms include sudden shortness of breath, chest pain, and dizziness, necessitating prompt medical intervention.
Other Essential Organs: Blood clots can also affect other vital organs, including the kidneys, intestines, and limbs. Kidney failure, bowel ischemia, and limb amputation can result from untreated clots in these areas, underlining the widespread threat posed by blood clots.
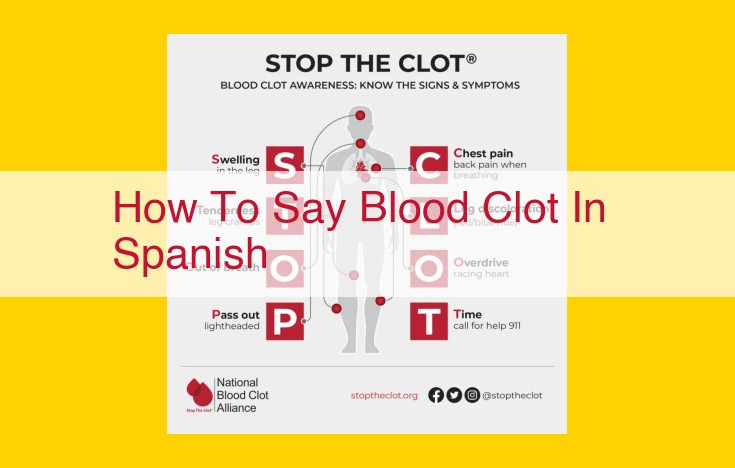
Local Symptoms: Recognizing the Inflammation’s Tale
If you experience discomfort in a specific part of your body, it could be a sign of a blood clot. In such cases, it’s essential to pay attention to the local symptoms, which often manifest themselves as inflammation.
The most common symptom of inflammation is swelling. The affected area may appear larger than usual due to fluid buildup. This swelling can be accompanied by discomfort and tightness.
Another typical symptom is pain. When blood flow is restricted by a clot, it can lead to pain and tenderness in the affected area. The severity of the pain can vary depending on the size and location of the clot.
Redness is another visible sign of inflammation. The affected area may appear flushed or discolored due to increased blood flow to the site of the clot.
Finally, inflammation is often associated with heat. The affected area may feel warmer to the touch compared to the surrounding areas. This is because inflammation triggers an increase in blood flow, leading to increased temperature.
Recognizing these local symptoms of inflammation is crucial as they can provide valuable clues about the presence of a blood clot. If you experience any of these symptoms, it’s important to seek medical attention promptly for proper assessment and treatment.
Systemic Symptoms of Blood Clots: A Warning Sign You Can’t Ignore
While local symptoms of blood clots, such as swelling and pain, can be alarming, it’s crucial to be aware of more severe systemic symptoms that may indicate a life-threatening condition. These symptoms warrant immediate medical attention.
Numbness and weakness in a limb or muscle group is a red flag that signals a possible deep vein thrombosis (DVT). This condition occurs when a blood clot forms in a deep vein, usually in the leg. If the clot breaks free and travels through the bloodstream to the lungs, it can cause a pulmonary embolism (PE), a potentially fatal condition.
Difficulty breathing is another serious symptom that should not be ignored. A blood clot in the lungs can block blood flow, making it hard to breathe. Chest pain, coughing up blood, and a rapid heart rate can also accompany a PE.
In some cases, blood clots can travel to the brain, causing a stroke. Symptoms of a stroke include sudden numbness or weakness on one side of the body, difficulty speaking or understanding speech, and vision problems.
If you experience any of these systemic symptoms, seek medical help immediately. Time is of the essence when it comes to treating blood clots, and early diagnosis and intervention can save lives.
Remember, prevention is key. By understanding the risk factors for blood clots and taking steps to reduce your risk, you can help protect yourself from this potentially life-threatening condition.
Modifiable Factors: Explain how age, obesity, smoking, hypertension, and diabetes increase the risk of thrombosis.
Modifiable Risk Factors for Blood Clots: A Preventable Threat
Certain lifestyle choices and health conditions can significantly increase your risk of developing blood clots. These modifiable factors, if addressed timely, can help reduce your chances of experiencing this potentially life-threatening condition.
> Age: As we grow older, our blood vessels become more prone to damage and inflammation. This can increase the likelihood of clot formation.
> Obesity: Excess weight strains the circulatory system, putting pressure on veins and impairing blood flow.
> Smoking: Nicotine damages the lining of blood vessels, making them more susceptible to clotting.
> Hypertension: High blood pressure forces blood through vessels at greater speed, increasing the risk of damage and clot formation.
> Diabetes: This condition leads to elevated blood sugar levels, which can damage blood vessels over time, making them more prone to clotting.
Recognizing and addressing these modifiable factors is crucial for minimizing your risk of blood clots. By implementing positive lifestyle changes and managing your health conditions effectively, you can take proactive steps towards preventing this potentially dangerous threat.
Non-Modifiable Factors: The Silent Contributors to Blood Clots
While certain lifestyle choices play a crucial role in the formation of blood clots, there are other factors that lie beyond our control. These non-modifiable factors can silently increase our risk of developing these potentially life-threatening events.
Genetics: The Invisible Hand
Genetics plays a significant role in the development of blood clots. Some individuals are born with inherited conditions that make their blood more prone to clotting. These conditions include Factor V Leiden and Prothrombin gene mutation, which increase the production of clotting factors.
Certain Medical Conditions: An Underlying Threat
Certain medical conditions can also increase the risk of blood clots. Cancer, especially pancreatic, lung, and ovarian cancer, releases substances that trigger blood clotting. Additionally, inflammatory conditions such as lupus, rheumatoid arthritis, and inflammatory bowel disease can also promote clotting by damaging blood vessels.
Prolonged Immobility: A Silent Risk
Extended periods of immobility, such as prolonged bed rest, long-distance travel, or certain medical procedures, can significantly increase the risk of blood clots. When you’re not moving, blood flow slows down, allowing clots to form more easily in the veins of the legs or pelvis.
Medications for Blood Clots: Unlocking the Power of Anticoagulants and Thrombolytics
When blood clots form, they can pose a serious threat to your health. They can block blood flow to vital organs, leading to strokes, heart attacks, or even death. Fortunately, there are medications that can help prevent and treat blood clots, giving you a fighting chance against their potentially devastating effects.
Anticoagulants: The Silent Protectors
Anticoagulants work by interfering with the blood’s clotting process, preventing clots from forming or growing. These medications are often used to prevent blood clots in people who are at high risk, such as those with a history of clots, heart disease, or certain medical conditions.
Thrombolytics: Dissolving the Threat
Thrombolytics are a different class of medications that work by dissolving existing blood clots. They are typically used to treat blood clots that have already formed and are blocking blood flow. Thrombolytics can be given intravenously or directly into the clot itself.
Working Together for Optimal Outcomes
In some cases, a combination of anticoagulants and thrombolytics may be used to maximize the effectiveness of treatment. Anticoagulants can help prevent new clots from forming while thrombolytics work to dissolve existing ones.
Understanding the Risks and Benefits
While medications can be a powerful tool in the fight against blood clots, it’s important to understand the risks and benefits involved. Anticoagulants can increase your risk of bleeding, while thrombolytics can cause side effects such as nausea, vomiting, or allergic reactions.
Talk to Your Doctor
If you have a blood clot or are at high risk of developing one, it’s crucial to talk to your doctor about the best medication options for you. They will assess your individual situation and recommend the best course of treatment to help you manage your condition and reduce your risk of future blood clots.
Surgical Interventions: Removing Blood Clots
In certain cases, blood clots may require surgical intervention to prevent or alleviate life-threatening consequences. Specialized surgical procedures, such as thrombectomy, play a crucial role in removing these dangerous clots.
Thrombectomy
Thrombectomy is a surgical procedure designed to remove blood clots from arteries or veins. This procedure is critical in situations where a clot is blocking blood flow to vital organs, such as the brain or heart.
During a thrombectomy, the surgeon makes a small incision and inserts a thin, flexible tube called a catheter into the affected blood vessel. The catheter is then guided to the location of the clot using X-ray imaging. Once the clot is reached, the surgeon uses a device attached to the catheter to break up and remove the clot.
Other Surgical Options
In some cases, additional surgical procedures may be necessary to treat blood clots. These procedures include:
-
Bypass surgery: Creating a new pathway for blood to flow around a blocked artery.
-
Endarterectomy: Removing the lining of an artery that has become narrowed or blocked by plaque.
-
Embolectomy: Surgically removing an embolus, a blood clot that has traveled through the bloodstream and blocked a blood vessel.
Role of Surgical Interventions
Surgical interventions for blood clots are crucial in life-threatening situations, such as:
-
Stroke: A blood clot in the brain that blocks blood flow, causing irreversible damage.
-
Heart attack: A blood clot in the heart’s arteries that blocks blood flow to the heart muscle.
-
Pulmonary embolism: A blood clot in the lungs that blocks blood flow, causing shortness of breath and chest pain.
Through surgical interventions, doctors can restore blood flow, prevent further damage, and save lives.
Lifestyle Modifications to Prevent Blood Clots
Blood clots, formed when blood thickens and clumps together, can pose significant risks to health. While certain risk factors are non-modifiable, adopting a healthy lifestyle can significantly reduce the chances of developing these dangerous clots. Here are several crucial lifestyle modifications that can help prevent blood clots:
Exercise Regularly
Physical activity is paramount in preventing blood clots. Exercise improves blood circulation, reduces the risk of obesity, and lowers blood pressure, all factors that contribute to clot formation. Aim for at least 30 minutes of moderate-intensity exercise most days of the week.
Manage Weight
Obesity increases the risk of blood clots by putting pressure on blood vessels and slowing down circulation. Maintaining a healthy weight can significantly reduce this risk. Focus on a balanced diet low in processed foods, sugary drinks, and unhealthy fats.
Quit Smoking
Smoking damages blood vessel walls, increases inflammation, and promotes the formation of blood clots. Quitting smoking is essential for reducing the risk of blood clots and improving overall health.
Other Lifestyle Adjustments
In addition to the above key modifications, other lifestyle adjustments can further minimize the risk of blood clots:
- Stay hydrated: Drink plenty of water to maintain proper blood flow.
- Avoid prolonged sitting or standing: Take frequent breaks to move around and prevent blood from pooling.
- Wear compression socks: These socks help improve circulation and reduce the risk of clots in the legs.
- Consider blood thinners: If you have a high risk of blood clots due to medical conditions or family history, your doctor may prescribe blood thinners to prevent clot formation.
Navigating Blood Clots: Essential Medical Precautions for Your Well-being
While some blood clots are not a cause for concern, others can pose significant risks to your health. For individuals at high risk of developing blood clots, taking precautionary measures is crucial to safeguard your well-being. Understanding the signs and symptoms of blood clots is the first step towards early detection and treatment.
Compression Stockings: A Supportive Guardian for Your Legs
Compression stockings are specially designed garments that exert gentle pressure on your legs, promoting blood circulation and preventing blood from pooling. They are particularly beneficial for individuals who spend prolonged periods sitting or standing, as these positions can increase the risk of blood clots in the legs.
Blood Thinners: Intervening at the Molecular Level
Medications known as blood thinners or anticoagulants can be prescribed to reduce the tendency of your blood to clot. These medications work by interfering with the clotting process, making it less likely for clots to form or grow. Blood thinners are often used in conjunction with other preventive measures, such as compression stockings.
Lifestyle Recommendations: Empowering You through Healthy Habits
In addition to medical precautions, embracing healthy lifestyle choices can significantly reduce your risk of developing blood clots. Regular exercise promotes blood flow and strengthens your vascular system, while maintaining a healthy weight minimizes pressure on your blood vessels. Quitting smoking is another crucial step, as nicotine can damage blood vessel walls and increase the risk of clots.
Seeking Professional Guidance for Peace of Mind
If you have any concerns about blood clots, it is essential to consult with your healthcare provider. They can assess your risk factors, recommend appropriate preventive measures, and provide personalized guidance to ensure your well-being. Early detection and treatment of blood clots can significantly improve your chances of a full recovery.
Empower Yourself with Knowledge and Care
By understanding the signs and symptoms of blood clots and taking the necessary precautionary measures, you can proactively safeguard your health. Compression stockings, blood thinners, and healthy lifestyle habits are powerful tools in your arsenal to prevent the development of blood clots. Remember, empowering yourself with knowledge and care is the key to a healthier and more fulfilling life.