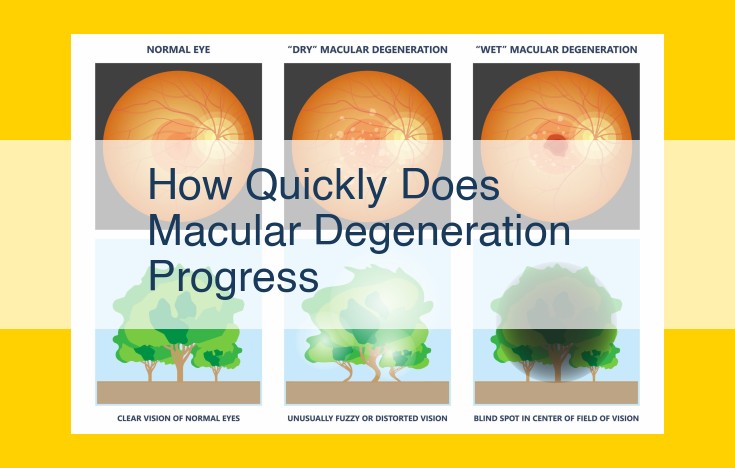
Macular degeneration progresses at variable rates, influenced by individual factors. Early dry AMD may remain stable for years, while advanced wet AMD can lead to rapid vision loss. Drusen, small yellow deposits in the retina, are early signs of AMD. As AMD progresses, drusen become larger and more numerous, leading to thinning of the macula and potential blind spot formation. In wet AMD, abnormal blood vessel growth under the retina causes swelling and leakage, resulting in rapid vision loss. The rate of progression from early dry AMD to advanced wet AMD varies significantly, making it crucial for regular eye exams to monitor disease progression and initiate timely treatment.
Understanding Age-Related Macular Degeneration (AMD)
Step into the Shadows of Aging Eyesight
Age-related macular degeneration (AMD) is a stealthy thief that silently robs us of our precious vision. As we journey through the corridors of time, our eyes, the windows to our souls, begin to show signs of wear and tear. AMD is a common eye condition that primarily affects the macula, the central part of the retina responsible for sharp, detailed vision.
A Silent Epidemic
With age as its relentless accomplice, AMD has become an alarmingly prevalent condition, casting a shadow over millions of aging populations worldwide. It is estimated that over 8 million Americans over the age of 50 suffer from AMD, making it a leading cause of vision loss in this age group.
Understanding Age-Related Macular Degeneration (AMD)
Age-related macular degeneration (AMD) is a common eye condition that affects millions worldwide. It primarily affects the macula**, a small, central area of the retina responsible for sharp, detailed vision**.
Causes of AMD
The exact causes of AMD are multifactorial, but several risk factors have been identified:
-
Age is the most significant risk factor. As we age, the macula undergoes degenerative changes.
-
Smoking is a major contributor to AMD. Chemicals in cigarettes damage the macula, increasing the risk of both dry and wet AMD.
-
Blue light exposure from electronic devices and sunlight can cause oxidative stress in the macula, damaging the light-sensitive cells and contributing to AMD.
-
Sunlight exposure emits ultraviolet radiation, which can harm the retina, especially if combined with other risk factors.
By understanding these risk factors, you can take proactive steps to reduce your susceptibility to AMD.
Early/Intermediate Dry AMD: Symptoms and progression
Early/Intermediate Dry AMD: A Journey of Vision Changes
As the years go by, the lens of our eyes gradually loses its flexibility, leading to a condition known as presbyopia, which manifests as difficulty focusing on nearby objects. However, age can also bring about a more serious eye-related concern: Age-Related Macular Degeneration (AMD).
AMD is a leading cause of vision loss in people over 50 years old. It affects the macula, a small, highly sensitive area in the center of the retina responsible for central vision, which is essential for activities such as reading, driving, and recognizing faces.
There are two main types of AMD: dry and wet. Early/Intermediate Dry AMD is the most common form, affecting approximately 90% of AMD cases. It progresses slowly over time, with gradual changes in vision that may go unnoticed initially.
As dry AMD advances, drusen, small yellow deposits, begin to accumulate in the macula. These drusen can disrupt the function of the macula, leading to symptoms such as:
- Blurred vision: Objects may appear less sharp or defined.
- Distorted vision (metamorphopsia): Straight lines may appear wavy or crooked, making it difficult to read or drive.
- Central blind spot: A small area in the central vision may become blurry or disappear altogether, affecting activities like reading and recognizing faces.
These symptoms can vary in severity and may not be immediately noticeable. However, as dry AMD progresses to intermediate stage, the changes in vision become more apparent. The drusen become larger and more numerous, and the pigment epithelium, a layer of cells beneath the macula that nourishes the photoreceptors, begins to deteriorate. This can lead to a gradual thinning of the macula, further compromising central vision.
Understanding the early and intermediate stages of dry AMD is crucial for timely diagnosis and treatment. Regular eye exams, especially after the age of 50, can help detect AMD in its early stages, allowing for appropriate interventions to preserve vision and maintain quality of life.
Advanced/Wet AMD: Rapid vision loss due to abnormal blood vessel growth
Advanced Wet Age-Related Macular Degeneration (AMD)
While many associate AMD with gradual vision loss, advanced wet AMD presents a more _alarming scenario_. This condition, characterized by _abnormal blood vessel growth_, threatens to _rapidly rob you of your sight_.
Imagine tiny, _fragile blood vessels_ sprouting beneath your retina, like rogue vines strangling a delicate flower. These _unruly vessels_ leak blood and fluid, casting a veil over your central vision. Initially, you may notice _slight blurring or distortions_, but as the condition progresses, _your sight can vanish_ before your very eyes.
This relentless form of AMD advances with alarming speed, _casting a shadow of fear_ over the present and future. However, _advanced wet AMD is not an inevitable fate_. With prompt diagnosis and timely treatment, there is hope for _preserving your precious eyesight_.
Geographic Atrophy (GA): Late stage with irreversible vision loss
Geographic Atrophy: The Irreversible Stage of AMD
At the end of the spectrum of Age-Related Macular Degeneration (AMD) lies Geographic Atrophy (GA), a late-stage and irreversible form characterized by the progressive loss of central vision.
GA occurs when light-sensitive cells in the macula, the central part of the retina responsible for sharp vision, gradually deteriorate. This deterioration leads to patches of thinned tissue that resemble geographic regions on an eye exam.
The precise cause of GA remains unknown, but it’s believed to involve a complex interplay between genetic, environmental, and age-related factors. Advanced age, smoking, and a family history of AMD are significant risk factors.
GA typically develops slowly, often going unnoticed during its early stages. As the condition progresses, individuals may experience:
- Blurred central vision: Objects appear hazy or out of focus.
- Altered color perception: Colors may become faded or washed out.
- Reduced contrast sensitivity: Difficulty distinguishing between light and dark areas.
- Blind spots: Central areas of vision gradually disappear.
Due to the irreversible nature of GA, treatment options primarily focus on slowing the progression and preserving residual vision. Anti-VEGF injections, laser therapy, and low-vision aids can help enhance mobility, reading, and other daily activities.
Living with GA presents its challenges, but with the right support and resources, individuals can adapt and maintain a meaningful quality of life. Sharing stories, connecting with support groups, and seeking professional advice can provide comfort and empowerment. Remember, even with the loss of central vision, there are still ways to thrive and embrace the world around us.
Family History: A Silent Shadow in the Battle Against AMD
When it comes to Age-Related Macular Degeneration (AMD), family history plays an enigmatic role, weaving its thread into the tapestry of this relentless condition. While age remains the most formidable risk factor, the inheritance we receive from our ancestors can silently increase our vulnerability to AMD’s devastating effects.
For those with a _family history of AMD_, the risk of developing the condition soars, signaling an increased likelihood of having the genetic predispositions that make their eyes more susceptible to the insidious progression of AMD. This inherited susceptibility resides within the intricate tapestry of our DNA, influencing the delicate mechanisms that protect our vision.
Yet, even within families touched by AMD, the web of genetics can be unpredictable. Some individuals may carry the torch of risk, while others remain unscathed. It’s a genetic roulette, where the odds shift depending on the specific genetic variations inherited from both parents.
Understanding your family history of AMD is a crucial step in safeguarding your vision. If you have close relatives who have been diagnosed with the condition, it’s imperative to consult an eye care professional. Regular eye examinations can detect early signs of AMD, empowering you to take proactive measures to mitigate its progression.
Obesity
3. Risk Factors for Developing AMD
Among the various risk factors that can increase your likelihood of developing Age-Related Macular Degeneration (AMD), obesity stands out as a significant contributor. Excess body weight puts strain on your body in many ways, and your eyes are no exception.
How Obesity Affects AMD
Obesity is associated with an increased risk of AMD due to several mechanisms:
- Chronic inflammation: Obesity fuels a state of chronic inflammation in the body, which can damage the delicate tissues of the macula.
- Oxidative stress: Obesity generates excessive free radicals, which contribute to oxidative stress and damage to the retinal cells.
- High blood pressure: Obese individuals often have high blood pressure, which can put stress on the blood vessels in the eye and lead to AMD.
- Altered blood sugar levels: Obesity can lead to insulin resistance and elevated blood sugar levels, which can also contribute to AMD.
Managing Obesity to Reduce AMD Risk
Maintaining a healthy weight is crucial for overall well-being and can significantly reduce your risk of developing AMD. Here are some tips for managing obesity:
- Adopt a balanced diet: Focus on consuming nutrient-rich foods such as fruits, vegetables, whole grains, and lean proteins.
- Engage in regular physical activity: Aim for at least 30 minutes of moderate-intensity exercise most days of the week.
- Consult a healthcare professional: If you struggle with weight management, seek guidance from a doctor or registered dietitian.
Remember, every pound lost can make a positive impact on your health, including your eye health. By addressing obesity, you empower yourself to take proactive steps towards reducing your risk of AMD and preserving your precious vision.
High Blood Pressure and Age-Related Macular Degeneration (AMD)
Age-Related Macular Degeneration (AMD) is a leading cause of irreversible vision loss in individuals over 50. While many factors contribute to the development of AMD, high blood pressure stands out as a modifiable risk factor that we can address to protect our eye health.
The Link Between High Blood Pressure and AMD
High blood pressure, also known as hypertension, puts excessive strain on the delicate blood vessels in the eyes. Over time, this strain can weaken and damage the blood vessels in the macula, the central part of the retina responsible for sharp central vision.
How High Blood Pressure Affects the Macula
The macula relies on a network of tiny blood vessels to nourish and oxygenate its cells. High blood pressure can cause these blood vessels to become narrowed, blocked, or even leak fluid into the surrounding tissue. This disruption of blood flow can lead to the formation of drusen, yellow deposits that are a hallmark of early AMD.
Impact on Vision
As AMD progresses, the damage to the macula can cause a range of vision problems, including:
- Blurred vision: The fine details of objects may appear fuzzy or unclear.
- Distorted vision (metamorphopsia): Lines may appear wavy or bent, and objects may seem smaller or larger than they actually are.
- Central blind spot: A dark area may develop in the center of vision, obscuring objects directly ahead.
Managing High Blood Pressure for Eye Health
Fortunately, controlling high blood pressure can significantly reduce the risk of developing AMD or slow its progression. Lifestyle changes, such as:
- Adopting a healthy diet low in sodium and saturated fat
- Engaging in regular physical activity
- Maintaining a healthy weight
- Quitting smoking, and
- Limiting alcohol intake
can all contribute to lowering blood pressure.
High blood pressure is a serious risk factor for AMD. By understanding its impact on the macula and taking steps to manage our blood pressure, we can proactively protect our vision and preserve our ability to see the world clearly.
High cholesterol
High Cholesterol and Age-Related Macular Degeneration (AMD)
In addition to the common risk factors for AMD, high cholesterol plays a significant role in the development of this debilitating eye disease. Cholesterol is a waxy substance that circulates in your blood and is essential for the body to function properly. However, high levels of cholesterol can lead to a buildup of fatty deposits in the blood vessels, including those of the retina.
These fatty deposits can restrict blood flow to the retina, depriving it of the oxygen and nutrients it needs to function properly. Over time, this can damage the delicate cells of the macula, the central part of the retina responsible for sharp central vision.
How High Cholesterol Contributes to AMD
- Plaque formation: High cholesterol can lead to the formation of plaque in the arteries, including those supplying blood to the eyes. This plaque can narrow or block the arteries, reducing blood flow to the retina.
- Inflammation: High cholesterol can trigger chronic inflammation in the body, which has been linked to the development and progression of AMD. Inflammation can damage the blood vessels in the retina and promote the formation of drusen, small yellow deposits that are associated with AMD.
- Oxidative stress: High cholesterol levels can contribute to oxidative stress, an imbalance between the production of free radicals and the body’s ability to neutralize them. Oxidative stress can damage the cells of the retina and accelerate the aging process.
Implications for Prevention and Management
Understanding the role of high cholesterol in AMD highlights the importance of managing cholesterol levels to reduce the risk of developing or progressing the disease. This can involve:
- Maintaining a healthy diet: A balanced diet low in saturated fat and cholesterol can help lower cholesterol levels. Include plenty of fruits, vegetables, whole grains, and lean protein.
- Getting regular exercise: Exercise helps improve blood circulation and may reduce cholesterol levels. Aim for at least 150 minutes of moderate-intensity exercise per week.
- Quitting smoking: Smoking increases inflammation and damages blood vessels, contributing to AMD. Quitting smoking can significantly improve your overall health and reduce your risk of AMD.
- Medications: If lifestyle changes are not enough to lower cholesterol levels, your doctor may prescribe medications such as statins or cholesterol absorption inhibitors.
Diabetes
Diabetes and Age-Related Macular Degeneration (AMD)
Age-related macular degeneration (AMD) is a leading cause of vision loss in older adults. Diabetes, a chronic condition that affects blood sugar levels, can increase the risk of developing AMD.
How Diabetes Affects AMD
High blood sugar levels associated with diabetes can damage the tiny blood vessels in the retina, the light-sensitive layer at the back of the eye. This damage can lead to the development of AMD, particularly the wet form, which is characterized by abnormal blood vessel growth under the retina.
Symptoms of AMD in Diabetics
The symptoms of AMD in individuals with diabetes may include:
- Blurry or distorted vision
- Difficulty seeing fine details
- Difficulty adapting to low light
- A central blind spot in the field of vision
Risk Factors
Diabetics have an increased risk of developing AMD due to several factors:
- Damage to blood vessels in the retina
- Inflammation
- Oxidative stress
- Nerve damage (neuropathy)
Management and Treatment
Managing blood sugar levels through diet, exercise, and medication is crucial to reduce the risk of developing AMD in diabetics. Regular eye exams are also essential for early detection and monitoring of AMD progression.
Treatment options for AMD in diabetics depend on the type and severity of the condition. These may include:
- Anti-VEGF injections: Inhibit blood vessel growth in the wet form of AMD
- Laser therapy: Seal leaking blood vessels
- Low-vision aids: Magnifying devices or special lighting to enhance vision for daily activities
Early diagnosis and treatment of AMD in diabetics can help preserve vision and maintain quality of life. Regular eye exams and adherence to diabetes management strategies are key to preventing and managing AMD in this population.
Understanding Blurred Vision: A Symptom of Age-Related Macular Degeneration (AMD)
Blurred vision, a common symptom of Age-Related Macular Degeneration (AMD), can be a disconcerting experience. AMD is a leading cause of vision loss in individuals over the age of 50, and it affects the macula, a small, central part of the retina responsible for sharp, central vision.
What Causes Blurred Vision in AMD?
Blurred vision in AMD typically occurs due to the accumulation of drusen, small yellow deposits in the macula. These deposits disrupt the normal functioning of the retinal cells, leading to blurred or distorted vision.
Early Signs and Progression
Initially, blurred vision may be mild and only noticeable in certain lighting conditions, such as low light. As AMD progresses, blurry areas may become more prominent and central, making it difficult to perform everyday tasks like reading, driving, or recognizing faces.
Advanced Stages of AMD
In advanced stages of AMD, the vision loss can become more severe. Some individuals may experience a central blind spot, known as geographic atrophy, where the macula’s cells are permanently damaged. This can lead to significant visual impairment and impact daily activities.
Seeking Medical Help
If you experience any changes in your vision, it’s crucial to seek medical attention promptly. An eye exam by an ophthalmologist can help diagnose AMD and determine the best course of treatment. Early detection and management can help preserve vision and prevent further deterioration.
Distorted Vision (Metamorphopsia): A Symptom of Age-Related Macular Degeneration (AMD)
In the realm of vision, metamorphopsia stands as a peculiar distortion, where objects appear warped, distorted, or even broken. This unusual visual phenomenon is often an early warning sign of Age-Related Macular Degeneration (AMD), a progressive eye condition that primarily affects the central vision.
AMD damages the macula lutea, a tiny area within the retina responsible for high-resolution central vision. As the disease progresses, the retinal pigment epithelium (RPE) supporting the macula can become damaged, leading to the formation of drusen: tiny yellow deposits that can disrupt the delicate balance of the macula.
When drusen accumulate, they can cause the macula to bulge or swell, resulting in distorted vision. Straight lines may appear wavy or broken, and objects can seem distorted or out of shape. This distortion can have a significant impact on daily activities such as reading, driving, or recognizing faces.
Metamorphopsia can be a subtle symptom, often mistaken for other vision issues such as nearsightedness or astigmatism. However, it’s essential to seek prompt medical attention if you experience any changes in your vision, especially if they are accompanied by other AMD symptoms like blurred central vision or difficulty adjusting to low light. Early detection and treatment can significantly improve the chances of preserving vision and maintaining a good quality of life.
Understanding Age-Related Macular Degeneration (AMD)
AMD is a leading cause of vision loss among seniors. It affects the macula lutea, a small area in the center of the retina responsible for sharp central vision. As we age, the macula undergoes changes that can affect its function, causing a distorted and blurry vision.
Central Blind Spot
One of the most noticeable symptoms of advanced AMD is the development of a central blind spot. This area of vision loss usually begins as a small, dark spot in the center of the visual field and can gradually expand over time. The central blind spot can make it difficult to read, drive, or recognize faces.
It is caused by damage to the macula’s cone cells, which are responsible for detecting light and color in the central part of vision. As the disease progresses, the cone cells become damaged and eventually die, resulting in a loss of function in the affected area.
The central blind spot can have a significant impact on daily activities. It can make it difficult to read, drive, or recognize faces. It can also make it difficult to see details in objects, such as the numbers on a clock or the words on a page.
If you notice a central blind spot or other changes in your vision, it is important to see a doctor right away. Early diagnosis and treatment can help to slow the progression of AMD and preserve vision.
Difficulty adjusting to low light
Difficulty Adjusting to Low Light: A Symptom of Age-Related Macular Degeneration (AMD)
As we age, we may experience difficulty adjusting to low-light conditions. While this can be a nuisance, it can also be a sign of Age-Related Macular Degeneration (AMD), a leading cause of vision loss in seniors. Understanding this symptom can help you seek timely diagnosis and management to protect your eye health.
The macula is a tiny area in the center of the retina responsible for our sharp, central vision. In AMD, the macula lutea becomes damaged, affecting our ability to see details clearly and adjust to low-light conditions. This is because the cells in the macula need adequate light to function properly. When light is insufficient, they struggle to send clear signals to the brain, resulting in blurred or distorted vision.
The inability to adapt to low light can significantly impact daily activities. You may find it challenging to drive at night, read in dimly lit areas, or participate in evening social events. This symptom can also increase your risk of falls and other accidents, as it affects your depth perception and balance.
If you’re experiencing difficulty adjusting to low light, it’s essential to seek professional evaluation. Your ophthalmologist will perform a comprehensive eye exam, including a Retinal Pigment Epithelium (RPE) and Macula Lutea examination, to check for signs of AMD. If AMD is diagnosed, early intervention is crucial to slow the progression of the disease and preserve your vision as much as possible.
Age-Related Macular Degeneration: Unveiling the Silent Thief of Sight
1. Understanding Age-Related Macular Degeneration (AMD)
Age-related macular degeneration (AMD) is an insidious eye condition that gradually steals vision, predominantly affecting individuals over 50. It’s the leading cause of severe vision loss in the elderly, impacting millions worldwide.
2. Types of AMD
AMD manifests in various forms:
- Dry AMD: The most common subtype, characterized by the accumulation of yellow deposits called drusen in the retina.
- Wet AMD: A more severe form that involves abnormal blood vessel growth in the macula, leading to rapid vision loss.
- Geographic Atrophy: End-stage AMD with irreversible vision loss due to degeneration of the central retina.
3. Risk Factors for Developing AMD
While aging is the primary risk factor, certain factors elevate the likelihood of developing AMD, including:
- Family history
- Obesity
- High blood pressure
- High cholesterol
- Diabetes
4. Symptoms of AMD
Early AMD often goes unnoticed, but as it progresses, symptoms may emerge:
- Blurry or distorted vision
- Central blind spot
- Difficulty adapting to low light
- Color distortion
5. Diagnosis of AMD
Retinal Pigment Epithelium (RPE) and Macula Lutea Examination:
The RPE and macula lutea are crucial structures in the retina responsible for central vision. During an eye exam, your doctor will meticulously examine these areas for abnormalities, such as:
- Drusen: Small yellow deposits that may indicate early AMD.
- Pigmentary changes: Alterations in the color pattern of the RPE, indicating disease progression.
- Abnormal blood vessels: Leaking or fragile vessels in wet AMD.
By closely scrutinizing the RPE and macula lutea, your doctor can accurately diagnose AMD and determine its severity.
**Understanding Age-Related Macular Degeneration (AMD): A Comprehensive Guide**
Age-related Macular Degeneration (AMD) is a leading cause of vision loss in people over 50. Understanding AMD is crucial for early detection and preserving vision.
Types of AMD
- Dry AMD: The most common form, with gradual vision loss over time.
- Wet AMD: A more severe form involving abnormal blood vessel growth in the eye, leading to rapid vision loss.
- Geographic Atrophy (GA): A late stage of AMD where the light-sensitive cells in the retina are destroyed, causing irreversible vision loss.
Risk Factors
- Age: The primary risk factor for AMD.
- Family history: Having a family member with AMD increases your risk.
- Smoking: Smokers have a significantly higher risk of developing AMD.
- Blue light exposure: Excessive exposure to blue light has been linked to an increased risk of AMD.
- Sunlight exposure: Long-term exposure to ultraviolet (UV) radiation from sunlight damages the retina.
- High blood pressure and cholesterol: These conditions can contribute to AMD development.
- Nutritional deficiencies: A diet low in fruits, vegetables, and vitamins C and E increases the risk.
Symptoms of AMD
- Blurred vision: Objects appear less clear than usual.
- Distorted vision (metamorphopsia): Straight lines may appear wavy or crooked.
- Central blind spot: A dark spot appears in the center of vision.
- Difficulty adjusting to low light: Vision may be impaired in dim lighting conditions.
Diagnosis
- Retinal Pigment Epithelium (RPE) and Macula Examination: Evaluates the health of the retina, including the macula.
- Drusen: Small Yellow Deposits in the Retina
Drusen are tiny, yellow deposits that form in the retina, particularly in people with AMD. Their presence is a clinical sign of the condition. As AMD progresses, drusen may increase in size and number, indicating the need for close monitoring and treatment.
Treatment Options
- Anti-VEGF Injections for Wet AMD: These injections inhibit the growth of abnormal blood vessels, preventing further vision loss.
- Laser Therapy: Seals leaking blood vessels in wet AMD.
- Low-Vision Aids: Enhance vision for activities of daily living, such as magnifying glasses or electronic devices.
AMD is a serious eye condition that can affect vision as we age. Understanding the risk factors, symptoms, and treatment options is essential for early detection and preserving vision. Regular eye exams, healthy lifestyle choices, and proper eye protection can help reduce the risk of developing AMD or slow its progression.
Understanding Anti-VEGF Injections: A Hopeful Treatment for Wet AMD
Wet age-related macular degeneration (AMD) is a progressive and sight-threatening condition that predominantly affects individuals over the age of 50. Unlike dry AMD, which progresses gradually, wet AMD is characterized by the growth of abnormal blood vessels behind the retina that leak fluid and blood, causing rapid and severe vision loss.
Fortunately, advancements in ophthalmic treatments have led to the development of anti-VEGF injections, which have revolutionized the management of wet AMD. These injections target a substance called vascular endothelial growth factor (VEGF), which plays a crucial role in the growth of new blood vessels. By blocking VEGF, anti-VEGF injections effectively inhibit the formation of these abnormal vessels, reducing fluid leakage and stabilizing vision.
The administration of anti-VEGF injections involves a simple, in-office procedure. The injections are typically administered directly into the vitreous humor, a clear gel-like substance in the back of the eye. The procedure is generally well-tolerated, with minimal discomfort or side effects.
The effectiveness of anti-VEGF injections in treating wet AMD has been well-established through extensive clinical trials. These trials have consistently demonstrated significant improvements in visual acuity, with many patients experiencing stabilization or even improvement in their vision. The injections also reduce the risk of further vision loss and preserve central vision, which is essential for activities like reading, driving, and recognizing faces.
For individuals diagnosed with wet AMD, anti-VEGF injections offer a beacon of hope. By effectively targeting the underlying cause of the condition, these injections provide a valuable treatment option to preserve vision and enhance quality of life. While regular injections are typically required to maintain the benefits, the significant vision-saving potential of anti-VEGF injections makes them a cornerstone of modern ophthalmic care. If you have been diagnosed with wet AMD, it is crucial to consult with your eye care professional to determine if anti-VEGF injections are right for you.
Laser Therapy: A Safe and Effective Treatment for Wet AMD
Age-related macular degeneration (AMD) is a leading cause of vision loss in older adults, affecting millions of people worldwide. While there is no cure for AMD, laser therapy offers a safe and effective treatment option for the wet form of the disease.
Wet AMD occurs when abnormal blood vessels grow underneath the retina, leaking fluid and blood. This can lead to rapid vision loss. Laser therapy aims to seal these leaking blood vessels and prevent further damage to the retina.
During laser therapy, a trained ophthalmologist uses a specialized laser to target the abnormal blood vessels. The laser emits a concentrated beam of light that heats and seals the blood vessel walls. This process is known as photocoagulation.
Photocoagulation can significantly reduce bleeding and fluid leakage, which can help preserve vision and slow the progression of the disease. Laser therapy is typically performed on an outpatient basis and requires multiple sessions over a period of time.
How Does Laser Therapy Work?
Laser therapy works by cauterizing the abnormal blood vessels. The laser light generates heat, which damages the blood vessel walls and seals them closed. This stops the leakage of fluid and blood, which can help prevent further damage to the retina.
The laser beam is precisely targeted to minimize damage to the surrounding healthy tissue. However, laser therapy may cause temporary side effects, such as blurred vision or floaters. These side effects usually subside over time.
Who is a Candidate for Laser Therapy?
Laser therapy is not suitable for all patients with wet AMD. It is most effective for people with early-stage wet AMD and those with specific blood vessel characteristics. Your ophthalmologist will assess your condition and determine if laser therapy is the right treatment option for you.
Benefits of Laser Therapy
Laser therapy has several benefits for people with wet AMD:
- Preserves vision: Laser therapy can help prevent further vision loss and preserve your current level of vision.
- Slows disease progression: By sealing the leaking blood vessels, laser therapy can slow down the progression of the disease and prevent further damage to the retina.
- Reduces bleeding and leakage: Laser therapy stops the bleeding and fluid leakage, which can improve vision clarity and reduce the risk of complications.
- Safe and effective: Laser therapy is a safe and effective procedure that has been used for decades to treat wet AMD.
Low-Vision Aids: Empowering Vision for Life’s Moments
When Age-Related Macular Degeneration (AMD) casts a shadow over vision, low-vision aids emerge as a lifeline. These innovative tools empower individuals to navigate everyday challenges and enhance their quality of life.
Magnifiers and Reading Aids:
Imagine the joy of reading your favorite book once more. Magnifiers come in various forms, from handheld devices to desktop models. They magnify printed text, making it easier for those with reduced central vision. Reading aids, such as page magnifiers and book stands, support comfortable reading experiences.
Optical Devices:
Telescopes are optical lifelines for those with diminished peripheral vision. These devices expand the field of view, allowing individuals to see objects that may otherwise be hidden from their sight. They can assist with activities like watching television or recognizing faces.
Mobility and Orientation Aids:
Navigating the world is essential for independence. Mobility canes and white canes help individuals with low vision to detect obstacles and move around safely. Orientation aids, such as GPS devices and sensory vests, provide environmental feedback and help with spatial awareness.
Assistive Technology:
Modern technology opens up a world of possibilities for those with low vision. Screen readers convert text to speech, enabling individuals to access digital information. Software and apps magnify text, enhance contrast, and offer other accessibility features.
The Emotional Impact:
The impact of low-vision aids extends beyond practical benefits. They provide hope, empowerment, and a sense of independence. When individuals can perform daily tasks and engage in meaningful activities, their spirits soar. Low-vision aids restore a sense of purpose and dignity.
In conclusion, low-vision aids are invaluable tools that light up the path for individuals with AMD. They enhance vision, boost confidence, and empower people to live their lives to the fullest. Embracing these aids is a powerful step towards reclaiming independence and maximizing potential.