The duration of tongue numbness after dental anesthesia depends on several factors, including the type of anesthesia used, the dosage, and the individual’s metabolism. On average, the numbness from local anesthesia, such as lidocaine, typically lasts for 2-4 hours, while regional anesthesia, such as a nerve block, can last for several hours to even days. The numbness may subside gradually as the anesthetic wears off, allowing sensation and movement to return to the tongue. However, it’s essential to follow the dentist’s instructions and avoid biting or chewing on the numbed area until sensation fully returns to prevent accidental injury.
Types of Dental Anesthesia: Understanding Your Options
When it comes to dental procedures, fear of pain often looms large. Fortunately, modern dentistry offers a range of anesthesia options to ensure a comfortable experience. Let’s explore the different types of dental anesthesia and their advantages and disadvantages:
Local Anesthesia: Numbing the Specific Area
Local anesthesia, also known as infiltration anesthesia, is the most commonly used technique. It involves injecting a numbing agent directly into the gum tissue surrounding the tooth being treated. This blocks nerve impulses, preventing the transmission of pain signals to the brain.
Advantages:
- Precise: Only the targeted area is numbed, allowing the patient to remain conscious and responsive.
- Quick-acting: Effects take place within minutes.
- Temporary: Numbness typically wears off within 1-2 hours.
Disadvantages:
- Short-lived: May not last long enough for extended procedures.
- Limited area: Only the injected area is numbed.
Regional Anesthesia: Blocking Nerves for a Wider Area
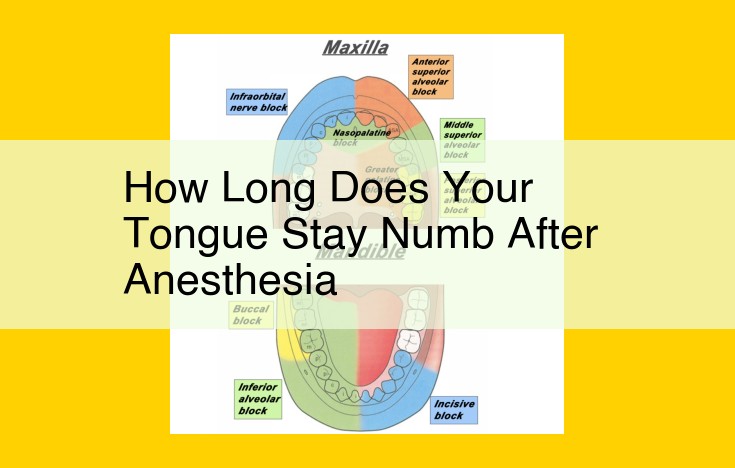
Regional anesthesia, also known as nerve block, involves injecting a numbing agent around a specific nerve to block pain signals from a larger area. Techniques include:
- Inferior alveolar nerve block: Numbs the lower jaw.
- Maxillary nerve block: Numbs the upper jaw.
- Gow-Gates mandibular block: Numbs the lower lip and chin.
Advantages:
- Broader area of numbness: Can numb multiple teeth or an entire jaw quadrant.
- Longer duration: Effects can last several hours.
- Good for lengthy procedures: Ensures comfort throughout the treatment.
Disadvantages:
- More complex to administer: Requires specialized training and experience.
- Can result in temporary numbness of the lips, tongue, or cheeks: Speech and eating may be affected.
General Anesthesia: Complete Unconsciousness
General anesthesia involves administering a combination of sedatives and pain relievers intravenously or through a mask. It renders the patient completely unconscious, blocking pain and awareness during the procedure.
Advantages:
- Painless experience: No discomfort or awareness during treatment.
- Suitable for complex procedures or anxious patients: Eliminates fear and allows for more extensive interventions.
- Long-lasting: Effects can last for several hours.
Disadvantages:
- Requires specialized equipment and anesthesiologist: Not readily available in all dental clinics.
- Risks of complications: Can include nausea, vomiting, and allergic reactions.
- Long recovery time: Requires a period of observation and recovery before the patient can be discharged.
Diving into the World of Dental Anesthetic Agents
When you step into the dentist’s chair, you may wonder about the magical elixir that will banish your dental discomfort. Enter anesthetic agents, the unsung heroes behind pain-free dental procedures. Let’s delve into the realm of these agents, exploring their types, characteristics, and how they work their wonders.
The Trio of Anesthetic Agents
In the dental armamentarium, there are three primary types of anesthetic agents:
-
Local Anesthesia: Confines its immobilizing effects to a specific area.
-
Regional Anesthesia: Targets nerves to numb a specific region, such as an entire jaw quadrant.
-
General Anesthesia: Induces unconsciousness, providing complete pain relief, and requires specialized monitoring.
Unveiling the Common Anesthetic Agents
Amongst the local anesthetic agents commonly used in dentistry, we have:
-
Lidocaine: A widely used agent known for its rapid onset, moderate duration, and safety profile.
-
Bupivacaine: A long-acting agent favored for procedures requiring extended numbness, but with a slower onset.
-
Ropivacaine: A long-acting agent similar to bupivacaine, offering less potential for cardiac toxicity.
-
Articaine: A unique agent that combines swift onset with a prolonged numbing effect, making it ideal for deeper procedures.
Understanding Their Mechanisms of Action
These agents work their magic by blocking nerve impulses that carry pain signals. They do so by interfering with the transmission of sodium ions through nerve cell membranes. By creating a barrier to ion flow, they disrupt the electrical signals that trigger pain sensations.
Side Effects: A Balancing Act
While these agents are generally safe, potential side effects include:
-
Local Reactions: Temporary swelling or tissue irritation.
-
Allergic Reactions: Though rare, allergic reactions can occur.
-
Systemic Effects: Rarely, agents can reach the bloodstream and cause effects such as drowsiness or dizziness.
The Importance of Informed Consent
Before administering any anesthetic agent, your dentist will carefully explain the procedure, potential benefits, and risks involved. This ensures you fully understand the anesthetic experience and can make an informed decision.
So, the next time you visit the dentist, rest assured that you are in capable hands. Anesthetic agents, with their diverse properties and mechanisms of action, play a crucial role in making your dental journey comfortable and pain-free.
Factors Influencing the Effectiveness of Dental Anesthesia
Understanding the various dental anesthesia techniques is crucial, but so is recognizing the factors that can impact their efficacy. These factors can determine the level of comfort and satisfaction you experience during your dental procedure.
Dosage and Concentration
The dose and concentration of the anesthetic used play a significant role in its effectiveness. A higher dose or concentration may provide deeper anesthesia, but it also increases the risk of side effects. Your dentist will determine the appropriate dose and concentration based on your individual needs and the type of procedure being performed.
Route of Administration
The route of administration refers to how the anesthetic is administered. Local anesthesia is typically injected into the tissues surrounding the affected area, while regional anesthesia involves injecting the anesthetic near a nerve to numb a larger area. General anesthesia is administered through inhalation or intravenously, resulting in a loss of consciousness. The choice of route depends on the extent of the procedure and your personal preferences.
Length of Exposure
The duration of anesthetic exposure also influences its effectiveness. Anesthetic agents typically have a finite duration of action. For longer procedures, additional doses may be required to maintain anesthesia. Your dentist will carefully monitor the duration of anesthesia to ensure optimal comfort throughout the procedure.
Patient Metabolism
Your body’s metabolism can affect how quickly the anesthetic is broken down and eliminated. Individuals with a faster metabolism may require higher doses or more frequent administrations. Your dentist will consider your metabolism when selecting the anesthetic and planning the dosage.
Presence of Infection
An ongoing infection can reduce the effectiveness of dental anesthesia. The presence of bacteria or inflammation can alter the pH of the tissues, affecting the absorption and distribution of the anesthetic. Your dentist may need to address the infection prior to administering anesthesia to ensure optimal results.
Patient Cooperation
Patient cooperation is essential for successful anesthesia administration. Following the dentist’s instructions, remaining still, and avoiding movement during injections can help ensure accurate placement of the anesthetic. Your dentist will provide clear instructions to guide you throughout the process.
Monitoring After Dental Anesthesia
After receiving dental anesthesia, it’s crucial to monitor patients closely to ensure their safety and well-being. This monitoring process involves assessing their nerve function, pain levels, and any potential complications that may arise.
Assessing Nerve Function
After the anesthesia wears off, it’s important to check the patient’s nerve function to ensure no damage has occurred. This can be done through a simple test that involves touching different areas of the mouth and asking the patient if they can feel the sensation. It’s also essential to observe the patient’s facial expressions for any signs of numbness or weakness.
Monitoring Pain
Evaluating the patient’s pain levels is also vital. This helps the dentist determine the effectiveness of the anesthesia and whether additional pain relief is necessary. Pain assessment can be done using a pain scale or by asking the patient to rate their discomfort level. It’s important to continue monitoring pain levels until they return to normal.
Managing and Preventing Complications
Although dental anesthesia is generally safe, there are some potential complications that can occur, including:
- Prolonged anesthesia: This can be managed by giving the patient time for the anesthesia to wear off or using a reversal agent.
- Nerve damage: This is a rare but serious complication that can occur if the anesthetic is injected incorrectly. It can lead to permanent numbness or weakness in the affected area.
- Infection: This can occur if the injection site is not properly sterilized. To prevent infection, the dentist will use sterile equipment and ensure the patient’s mouth is clean before administering the anesthesia.
Monitoring patients after dental anesthesia is essential to ensure their safety and comfort. By assessing nerve function, pain levels, and potential complications, dentists can promptly address any issues that arise. This monitoring process helps prevent and manage complications, ensuring that patients have a positive dental experience.