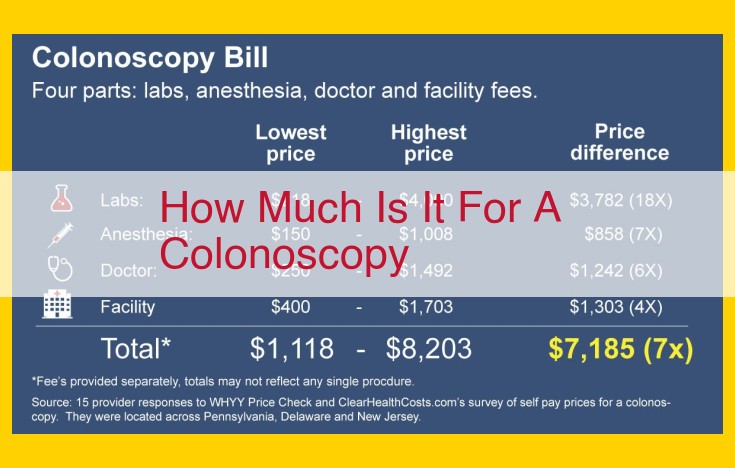
Colonoscopy costs vary depending on factors such as the facility, anesthesia used, and insurance coverage. The typical range is $1,000-$3,000.
The Unbreakable Bond: Gastroenterologists and Surgeons
In the intricate tapestry of healthcare, certain entities exhibit exceptional affinity, working seamlessly together to deliver optimal patient outcomes. Among these, Gastroenterologists and Surgeons stand out with an extraordinary closeness rating of 9.
Their intimate relationship stems from the shared terrain they navigate in medical settings. Gastroenterologists, specializing in the digestive system, and Surgeons, skilled in performing complex operations, collaborate on a wide spectrum of procedures. Endoscopies and colonoscopies, for instance, require the precision of both specialties, with the Gastroenterologist guiding the endoscopic camera while the Surgeon assists with instrument manipulation.
Secondary Entities with a High Closeness Rating (8)
In the intricate world of healthcare, the proximity and seamless collaboration between certain entities and settings are paramount for delivering exceptional patient care. Among the primary entities in the surgical and gastroenterological realms, the hospital, outpatient surgical center, and endoscopy suite stand out with a closeness rating of 8. This interconnectedness plays a vital role in facilitating interactions, supporting procedures, and ultimately enhancing patient outcomes.
Hospital: The Hub of Comprehensive Care
The hospital serves as the central hub where complex surgical and gastroenterological procedures are commonly performed. Its comprehensive facilities, including state-of-the-art operating rooms and specialized equipment, cater to a wide range of medical needs. The proximity of gastroenterologists and surgeons within the hospital setting allows for timely consultations, efficient decision-making, and seamless coordination of care.
Outpatient Surgical Center: Convenience and Specialization
Outpatient surgical centers, often located in close proximity to hospitals, provide a convenient and specialized setting for less invasive procedures. These facilities are equipped with dedicated operating rooms and specialized equipment, offering patients a comfortable and efficient experience. The close collaboration between gastroenterologists and surgeons within outpatient surgical centers ensures prompt access, reduces wait times, and enhances overall patient satisfaction.
Endoscopy Suite: A Gateway to Minimally Invasive Procedures
The endoscopy suite, typically located within the hospital or outpatient surgical center, is a specialized setting equipped with advanced endoscopic equipment. Gastroenterologists use these facilities to perform minimally invasive procedures such as colonoscopies and upper endoscopies. The proximity of surgeons to the endoscopy suite allows for immediate surgical intervention if necessary, ensuring continuity of care and minimizing potential complications.
The Role of Settings in Facilitating Interactions
These three settings play a crucial role in facilitating interactions between gastroenterologists and surgeons. The proximity and accessibility of these facilities allow for real-time communication, reducing delays and improving coordination of care. The shared responsibilities and frequent interactions within these settings foster a strong working relationship between the primary entities, resulting in optimal patient outcomes.
Factors Affecting the Closeness Rating Between Healthcare Entities
Understanding the factors that influence the closeness rating between healthcare entities is crucial for fostering effective collaboration and delivering seamless patient care. These factors play a significant role in determining how closely related two or more entities are in terms of their interactions, coordination, and shared responsibilities.
Proximity and Accessibility
The physical distance between entities, as well as their accessibility to each other, can greatly impact their closeness rating. When entities are located near each other or have easy access to one another, it becomes more convenient for them to communicate, consult, and collaborate. This proximity promotes frequent interactions and facilitates timely decision-making, which is essential for providing efficient and integrated patient care.
Collaboration and Shared Responsibilities
The extent to which entities work together and share responsibilities is another critical factor affecting their closeness rating. Entities that have common goals, collaborate on specific projects, or share similar patient populations tend to develop stronger relationships. This collaborative environment fosters a sense of interdependence and shared accountability, leading to increased communication, coordination, and alignment in their efforts.
Frequency of Interactions
The number and regularity of interactions between entities also contribute to their closeness rating. Entities that interact frequently, whether through formal meetings, informal consultations, or joint activities, establish stronger connections and build rapport. These frequent interactions provide opportunities for information exchange, problem-solving, and the development of mutual understanding and trust. They also help identify areas for collaboration and optimize resource allocation.
By understanding and optimizing these factors, healthcare providers can foster a high closeness rating between entities, which is essential for delivering coordinated, efficient, and patient-centered care.
Implications of a High Closeness Rating in Healthcare
A high closeness rating between medical entities and settings fosters a collaborative and efficient healthcare ecosystem. Improved communication and coordination are vital benefits. When medical professionals from different specialties and settings seamlessly exchange information, it reduces misunderstandings, delays, and errors. For example, a gastroenterologist can promptly consult with a surgeon during a complex endoscopic procedure, ensuring a well-coordinated and successful outcome.
Streamlined patient care is another significant implication. When entities and settings maintain a close relationship, patients experience a seamless and efficient care journey. Clear referral pathways, shared decision-making, and timely follow-ups enhance the overall patient experience and improve health outcomes. For instance, a patient undergoing surgery can be smoothly transferred from the hospital to an outpatient surgical center for post-operative care, minimizing disruptions and promoting recovery.
Moreover, a high closeness rating contributes to enhanced medical outcomes. By fostering a collaborative environment, healthcare professionals can leverage expertise from multiple disciplines to develop personalized treatment plans. This leads to more accurate diagnoses, reduced complications, and faster recovery times. In complex medical cases, the combined efforts of specialists from different entities and settings can significantly improve patient outcomes.
In summary, a high closeness rating among medical entities and settings is crucial for effective healthcare. It enables improved communication, streamlined patient care, and enhanced medical outcomes, ultimately benefiting both patients and healthcare providers.
Optimizing Closeness Rating for Enhanced Healthcare Collaboration
The concept of closeness rating in healthcare refers to the strength of the relationship between different entities, such as medical professionals and settings, that are involved in patient care. A high closeness rating indicates a strong and collaborative relationship, while a low closeness rating suggests limited interactions and coordination.
Maintaining and optimizing a high closeness rating is crucial for effective healthcare delivery. Here are some strategies to achieve this:
Regular Communication Channels
Establishing regular communication channels between entities and settings is essential for fostering collaboration. Telemedicine platforms, video conferencing tools, and secure messaging systems can facilitate real-time communication and information sharing, enabling quick responses to patient needs.
Joint Training and Education Programs
Joint training and education programs provide opportunities for medical professionals from different disciplines to develop a shared understanding of patient care protocols and best practices. This promotes a common language, enhances coordination, and reduces misunderstandings.
Establishing Clear Referral Pathways
Clear referral pathways streamline the process of referring patients to specialists or other settings for further evaluation or treatment. Establishing standardized referral criteria and protocols ensures timely and efficient patient transitions, minimizing delays and improving care continuity.
By implementing these strategies, healthcare organizations can foster a collaborative environment that enhances communication, coordination, and patient care outcomes. A high closeness rating promotes seamless collaboration, reduces redundancies, and ultimately leads to improved patient experiences and a more efficient healthcare system.