Buckle fractures, common in children, affect the outer layer of a bone. Healing typically takes 4-6 weeks, depending on the individual’s condition and the severity of the fracture. Immobilization is crucial to maintain stability during healing, allowing for the natural growth and repair processes to restore the bone to its original strength.
Understanding Bone Fractures: A Comprehensive Guide
Bone fractures are a common occurrence, affecting people of all ages and walks of life. Understanding the nature of these injuries is crucial for effective treatment and recovery. In this blog post, we will delve into the world of bone fractures, exploring their definition, different types, and the intricate mechanisms that drive their healing.
What is a Bone Fracture?
A bone fracture occurs when an excessive force is applied to a bone, causing it to break or crack. Fractures can range in severity from minor hairline cracks to complete breaks that extend through the entire thickness of the bone. The type of fracture depends on several factors, including the magnitude and direction of the force, bone density, and the structural characteristics of the bone itself.
Types of Bone Fractures
Bone fractures can be classified into various types based on their appearance, location, and severity. Some common types of fractures include:
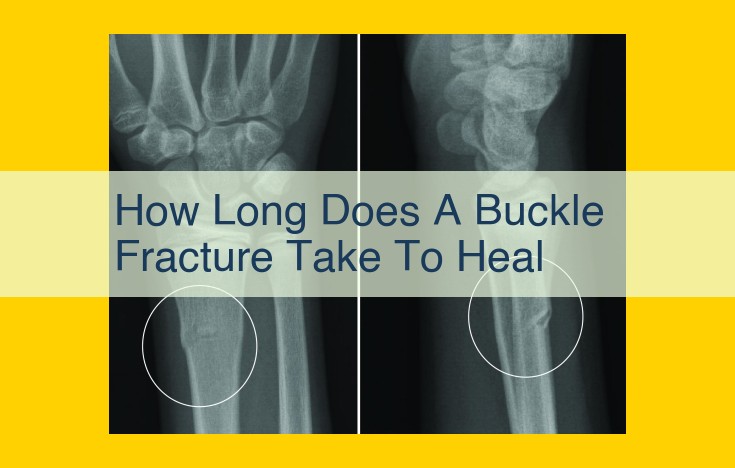
- Buckle fractures: Minor fractures that cause a bending or buckling of the bone without breaking it completely.
- Greenstick fractures: Incomplete fractures where one side of the bone is broken while the other side remains intact.
- Transverse fractures: Fractures that run perpendicular to the long axis of the bone.
- Oblique fractures: Fractures that run diagonally across the bone.
- Spiral fractures: Fractures that occur when the bone is twisted.
- Comminuted fractures: Fractures in which the bone is broken into multiple pieces.
Bone Growth and Repair: A Journey of Renewal
Our bodies are marvels of engineering, constantly adapting and repairing to keep us moving and thriving. When it comes to our bones, this intricate process is even more remarkable. Growth plates, cartilage, and bone remodeling play a vital role in creating and maintaining the strength and resilience of our skeletal system.
Growth Plates: Guiding Bone Length
During youth, our bones are adorned with growth plates, thin layers of cartilage located near the ends. These plates act as command centers, directing the growth and elongation of bones. As we age, these plates gradually close, marking the end of our skeletal growth spurt.
Cartilage: The Foundation for Bone
Cartilage, a flexible and supportive tissue, provides the blueprint for bone formation. It forms the initial mold for new bones during development and plays a role in bone repair. Cartilage cells, called chondrocytes, secrete a matrix of proteins and sugar molecules, which gives cartilage its unique properties.
Bone Remodeling: A Continuous Cycle of Renewal
Throughout our lives, our bones undergo a continuous cycle of bone remodeling. Specialized cells known as osteoclasts break down old bone tissue, while osteoblasts create new bone. This delicate balance ensures that our bones remain strong and adaptable, adjusting to mechanical stresses and wear and tear.
As we age, the rate of bone remodeling slows down, which can lead to a decrease in bone density and an increased risk of fractures. Understanding these mechanisms is crucial for maintaining bone health and reducing the risk of bone-related issues as we grow older.
Fracture Treatment: Immobilization Methods
Bone fractures are a common occurrence, affecting individuals of all ages. When a fracture occurs, the priority is to stabilize the injured area and promote healing. Immobilization methods play a crucial role in this process by holding the fractured bones in place, allowing them to knit together properly. This can help reduce pain, prevent further damage, and facilitate faster recovery.
The choice of immobilization method depends on the severity and location of the fracture. Splints and casts are the most common forms of immobilization. Splints are typically used for less severe fractures or temporary stabilization before a cast can be applied. They are made of a flexible material, such as fiberglass or plaster, that can be molded to fit the injured area.
Casts are rigid devices that fully immobilize the injured area. They are typically made of plaster or fiberglass and are applied by a healthcare professional. Casts provide more support and stability than splints and are used for more severe fractures.
Proper immobilization is essential for successful fracture healing. It ensures that the fractured bones are aligned correctly and stay in place, allowing them to heal without interference. Following the instructions provided by your healthcare provider regarding the use and care of your immobilization device is crucial to maximize healing outcomes.
The Journey of Bone Healing: Unraveling the Stages of Fracture Repair
When you experience a bone fracture, your body embarks on a remarkable healing journey that involves a complex interplay of biological processes. This journey unfolds in three distinct stages:
1. Inflammatory Phase:
- Immediately following the fracture, your body triggers an inflammatory response to protect the injured area.
- Blood vessels rush to the site, delivering oxygen and nutrients.
- Immune cells remove damaged tissue and prepare for healing.
2. Repair Phase:
- Soft tissue forms a blood clot that stabilizes the fracture fragments.
- Bone cells*, known as **osteoblasts, begin to lay down new bone tissue.
- Over several weeks, the new bone gradually bridges the fracture.
3. Remodeling Phase:
- Once the fracture heals, your body begins to remodel the repaired bone.
- Osteoblasts continue to add new bone, while osteoclasts remove old bone.
- This process shapes the bone back to its original form and restores its strength.
Throughout this journey, your body’s natural healing abilities, age, fracture severity, and overall health play crucial roles in determining the healing timeline. While a typical fracture may take 4-6 weeks to heal, more complex fractures may require 6-8 weeks or longer.
By understanding the stages of fracture healing, you can gain a deeper appreciation for your body’s resilience and the remarkable process of bone repair.
Timeline for Fracture Healing:
- Typical healing times (e.g., 4-6 weeks or 6-8 weeks)
Timeline for Fracture Healing: A Journey of Restoration
While every fracture is unique, understanding the general timeline of healing can provide a sense of comfort during the recovery process. Fracture healing often occurs in stages, each with its distinctive characteristics.
Phase 1: Inflammation
Immediately following a fracture, the body initiates an inflammatory response to protect the injured area. Blood vessels dilate, bringing immune cells and nutrients to the site. This initial phase typically lasts 2-3 days.
Phase 2: Repair
During the repair phase, the body begins to build new bone tissue. Cartilage cells, known as chondroblasts, form a callus that bridges the fracture gap. Over time, this cartilage callus undergoes a process called endochondral ossification, gradually replacing it with bone. This phase generally occurs within the first 2-4 weeks.
Phase 3: Remodeling
In the final remodeling phase, the newly formed bone remodels to restore its original shape and strength. The callus gradually disappears, and the bone regains its normal structure and density. This process can take several months or even years.
Typical Healing Timelines
The time it takes for a fracture to heal depends on several factors, including the severity of the injury, the location of the fracture, and the individual’s overall health. However, here are some general guidelines:
- Simple fractures: These fractures often heal within 4-6 weeks.
- Complex fractures: Fractures that involve multiple bone fragments or those that require surgery may take 6-8 weeks or longer to heal.
- Severe fractures: Fractures that involve significant bone loss or damage to nearby soft tissues can take several months or even years to heal.
It’s important to note that these healing times are approximate estimates. Always consult with your healthcare provider for personalized information and guidance on your specific fracture and its expected healing timeline.
Factors Influencing Fracture Healing:
- Age, fracture severity, immobilization duration, underlying health conditions, nutritional status, physical activity levels
Factors Influencing the Symphony of Fracture Healing
Fracture healing is a complex and often overlooked process that plays a pivotal role in our journey back to mobility. While age and the severity of the fracture inevitably hold sway, several other factors dance gracefully or clumsily with time to determine the orchestration and tempo of this healing symphony.
Age: The Graceful Waltz of Time
As time gracefully winds its tapestry, our bodies undergo a symphony of changes. In younger individuals, the bones exhibit a youthful exuberance, hosting an abundance of growth plates, vital for bone growth and repair. Imagine these growth plates as eager apprentices, swiftly weaving new bone tissue to heal fractures with remarkable efficiency.
However, as we journey through the seasons of life, our growth plates retire, and the bones lose some of their youthful vigor. This transition slows the healing process, requiring a more patient waltz with time.
Fracture Severity: The Forceful Crescendo
The severity of a fracture can dramatically alter the healing trajectory. Imagine a mere hair crack in a bone, resembling a whisper in the musical composition. Such fractures often heal swiftly, with the body’s natural repair mechanisms deftly mending the break with minimal fanfare.
However, when the fracture erupts into a loud crescendo, as in a complex break or displacement, the healing symphony becomes far more intricate. The body’s instruments must work in meticulous harmony to restore the bone to its former glory, requiring a more prolonged and demanding performance.
Immobilization Duration: A Delicate Balance
Immobilization, like a necessary pause in a musical composition, provides the ideal environment for bone healing. While a brief rest allows the fractured bone to mend, prolonged immobilization can introduce a dissonant note.
Imagine bones as dancers held motionless for too long. Their muscles atrophy, and their mobility becomes compromised. This immobility can impede the healing process, making it crucial to find the delicate balance between providing stability and allowing gentle movement to facilitate recovery.
Underlying Health Conditions: The Silent Discord
Underlying health conditions can subtly alter the rhythm of fracture healing. Conditions like diabetes, osteoporosis, and vascular disease can disrupt the harmonious flow of blood and nutrients to the injured bone, impairing its ability to repair itself.
These silent discords within the body’s symphony can prolong the healing process and make it more challenging to achieve a complete recovery.
Nutritional Status: The Vital Nourishment
As in any symphony, the nourishment provided to the healing bone is of paramount importance. A well-balanced diet, rich in calcium, vitamin D, and other essential nutrients, acts as the vital sustenance for bone repair. Without these building blocks, the bone’s ability to regenerate and strengthen is diminished, leading to a faltering healing process.
Physical Activity Levels: The Gentle Conductor
While complete immobilization can hinder healing, gentle physical activity can act as a subtle conductor, guiding the bone back to its former strength and flexibility. Moderate exercise stimulates blood flow to the injured area, delivering nutrients and oxygen to facilitate repair.
However, excessive or strenuous activity can strain the healing bone, disrupting its delicate balance and prolonging the healing journey. Finding the optimal balance between rest and rehabilitation is crucial for a harmonious symphony of recovery.