Blood Thinner Management for Dental Surgery
The duration of blood thinner stoppage before tooth extraction depends on the type of blood thinner. For warfarin, it may be up to 5 days; for aspirin, 3-7 days; for clopidogrel, 5-7 days; and for direct oral anticoagulants (DOACs) like dabigatran or rivaroxaban, 1-2 days. The specific timeframe is determined by the individual patient’s risk of bleeding and clotting, as well as the dental procedure being performed.
Blood Thinner Management for Dental Surgery: Minimizing Risks
Before undergoing dental surgery, it’s paramount to assess both bleeding and thromboembolic risks. These factors are crucial in determining the safest approach to managing blood thinners during the procedure.
Bleeding Risk
The type of dental procedure plays a significant role in bleeding risk. Minor procedures like check-ups or fillings usually pose minimal risk, while more invasive surgeries like tooth extractions or implants may increase the likelihood of bleeding. A patient’s medical history is also a key consideration. Conditions that impair blood clotting or cause excessive bleeding, such as hemophilia or thrombocytopenia, warrant closer monitoring.
Thromboembolic Risk
Certain factors can increase the patient’s thromboembolic risk, namely their age. Older patients are more likely to develop thromboembolisms, or blood clots. Comorbidities like coronary artery disease, stroke, and atrial fibrillation also contribute to this risk. Genetic predispositions, such as inherited thrombophilia disorders, further elevate the patient’s susceptibility to clots.
Blood Thinner Management for Dental Surgery: Understanding the Risks and Strategies
Before embarking on any dental procedure, it’s crucial to understand the potential risks associated with blood thinners and the strategies available to manage them. Blood thinners, also known as anticoagulants and antiplatelet drugs, are medications prescribed to prevent or treat blood clots. However, they can also increase the risk of bleeding during dental surgery.
Factors Influencing Bleeding Risk
Several factors can influence the risk of bleeding during dental surgery in patients taking blood thinners. The type of dental procedure is a primary consideration. Procedures involving soft tissue manipulation, such as gum surgery or tooth extraction, carry a higher bleeding risk compared to procedures like fillings or cleanings.
The patient’s medical history also plays a significant role. Conditions such as liver disease, kidney disease, or recent surgery can increase the likelihood of bleeding. Additionally, medications other than blood thinners, such as anti-inflammatory drugs or aspirin, can further contribute to bleeding risk.
A thorough understanding of these factors is essential for healthcare professionals to assess the bleeding risk accurately and develop appropriate management strategies.
Blood Thinner Management: A Journey for Safe Dental Surgery
Prologue: The Patient’s Dilemma
For patients taking blood thinners, dental surgery can present a unique challenge. These medications are essential for preventing life-threatening blood clots, but they can also increase the risk of bleeding during invasive procedures. Fortunately, with careful planning and collaboration, dental surgery can be performed safely and effectively, ensuring a positive outcome.
Assessing the Risks: A Balancing Act
Before embarking on any dental procedure, a comprehensive risk assessment is crucial. Bleeding risk is influenced by factors such as the type of surgery planned and the patient’s medical history. Conditions like thrombocytopenia, liver disease, or recent bleeding events may warrant extra precautions.
Thromboembolic risk is also a concern. As we age, our blood’s tendency to clot increases. Certain comorbidities, such as diabetes or heart disease, further elevate this risk. Genetic predispositions, like thrombophilia, add another layer of complexity.
Know Your Medication: A Variety of Blood Thinners
Patients taking blood thinners may be prescribed anticoagulants or antiplatelet drugs. Anticoagulants, such as warfarin or heparin, target the clotting cascade, while antiplatelet drugs, like aspirin or clopidogrel, prevent platelet aggregation. Understanding the mechanism of action of each medication is essential for devising a tailored management plan.
Dental Procedures: Understanding the Bleeding Risk
Common dental procedures, like tooth extraction, dental surgery, and oral surgery, may carry varying degrees of bleeding risk. Tooth extraction, for instance, typically involves more bleeding than a routine cleaning. Dentists must be aware of the patient’s blood thinner regimen to minimize the potential for complications.
Blood Thinner Management for Dental Surgery: A Guide for Patient Safety
Dental procedures are essential for maintaining oral health, but they can pose unique challenges for patients taking blood thinners. Understanding the risks and developing a tailored management plan is crucial to ensure a safe and successful experience.
Blood Thinners: Types and Effects
Blood thinners are medications that reduce clotting to prevent or treat blood clots. They fall into two main categories:
-
Anticoagulants: Warfarin (Coumadin), heparin, and dabigatran (Pradaxa) interfere with the blood’s clotting factors.
-
Antiplatelet drugs: Aspirin, clopidogrel (Plavix), and prasugrel (Effient) prevent platelets from forming blood clots.
Dental procedures, such as tooth extractions and surgeries, can increase the risk of bleeding. Conversely, stopping blood thinners abruptly can raise the risk of dangerous blood clots.
Risk Assessment: Balancing Bleeding and Clot Risks
Before any dental surgery, assessing the patient’s bleeding and thromboembolic (blood clot) risks is paramount.
-
Bleeding risk: Factors include the type of dental procedure, the patient’s medical history (e.g., anemia, bleeding disorders), and the specific blood thinner being used.
-
Thromboembolic risk: Age, certain medical conditions (e.g., heart disease, diabetes), and genetic predispositions can increase the likelihood of blood clots.
Collaboration of Healthcare Professionals
Managing blood thinners for dental surgery requires a team effort:
-
Physician (prescribing doctor): Determines the appropriate blood thinner and manages the patient’s overall medical condition.
-
Dentist (performing surgery): Evaluates the surgical risk and develops a plan to minimize bleeding.
-
Pharmacist (dispensing medications): Provides medication counseling and monitors drug interactions.
Clear communication and coordination among these professionals is vital for optimal patient care.
Blood Thinner Management: A Guide for Safer Dental Surgery
When preparing for dental surgery, patients taking blood thinners face a unique set of challenges. To ensure their safety, a collaborative approach involving physicians, dentists, and pharmacists is crucial. Understanding the risks and management strategies of blood thinners is paramount for both healthcare professionals and patients alike.
Assess the Risks
Before any dental procedure, it is essential to assess both bleeding and thromboembolic risks. Factors that influence bleeding risk include the type of procedure and the patient’s medical history, such as past bleeding episodes, liver disease, or certain medications. Thromboembolic risk is influenced by age, comorbidities like heart disease or stroke, and genetic predispositions.
Entities Involved
Blood Thinners
Various types of blood thinners are used:
- Anticoagulants: Prevent blood clots by interfering with their formation. Examples include warfarin and heparin.
- Antiplatelet Drugs: Inhibit platelet function, preventing them from clumping together. Examples include aspirin and dabigatran.
Dental Procedures
Common dental procedures that require blood thinner management include:
- Tooth extractions
- Dental implants
- Oral surgery
The bleeding risk associated with each procedure varies, and healthcare professionals will consider this when making management decisions.
Healthcare Professionals
Interdisciplinary collaboration is vital. The physician prescribing the blood thinner, the dentist performing the surgery, and the pharmacist dispensing the medications all play crucial roles. Clear communication and shared decision-making ensure the safety of the patient.
Management Strategies
Approaches to manage blood thinners before and after dental surgery vary:
- Platelet Transfusions: Increase platelet count to enhance clotting ability.
- Antifibrinolytic Drugs: Prevent clot breakdown, reducing bleeding risk.
- Thromboembolic Risk Reduction: Use of compression stockings, early ambulation, and other measures to prevent blood clots.
Patient Education and Informed Consent
Educating patients about the risks and benefits of blood thinner management is essential. They should understand their responsibilities in following instructions, monitoring for complications, and reporting any concerns promptly. Informed consent ensures patients are fully aware of the potential implications of their treatment decisions.
Blood thinner management for dental surgery requires a comprehensive approach considering individual patient risks, procedure-specific concerns, and collaborative healthcare efforts. By following established guidelines and empowering patients with knowledge, we can optimize dental care for those taking blood thinners, ensuring their safety and well-being.
Blood Thinner Management for Dental Surgery: A Guide for Understanding and Managing Risks
When it comes to dental surgery, understanding the risks and benefits of blood thinners is crucial. As a patient taking blood thinners, it’s essential to engage in open communication with your healthcare team for proper management before, during, and after your procedure.
Understanding the Mechanisms of Blood Thinners
Blood thinners, including anticoagulants and antiplatelet drugs, play a vital role in preventing blood clots.
- Anticoagulants, such as warfarin, heparin, and dabigatran, interfere with the body’s clotting cascade, slowing down the formation of blood clots.
- Antiplatelet drugs, such as aspirin and clopidogrel, inhibit platelet aggregation, reducing the ability of platelets to form a clot.
Collaborative Approach: Involving Healthcare Professionals
Effective management of blood thinners for dental surgery requires a team effort among the physician, dentist, and pharmacist.
- Physician: Assesses bleeding and thromboembolic risks, prescribes blood thinners, and provides overall guidance.
- Dentist: Performs the dental procedure, assesses potential bleeding risks, and monitors for complications.
- Pharmacist: Dispenses blood thinners, educates patients on medication use, and monitors for drug interactions.
By working together, these healthcare professionals ensure a coordinated and safe approach to your dental care.
Blood Thinner Management for Dental Surgery: A Guide for Patients
Assessing Your Risk
Before embarking on dental surgery, it’s crucial to evaluate your bleeding and thromboembolic risks. Your dental procedure, medical history, and personal circumstances all play a role. Dental procedures that involve cutting or removing tissue, such as tooth extraction, dental implant placement, and root canal treatment, necessitate closer monitoring.
Common Blood Thinners and Their Mechanisms
Blood thinners, also known as anticoagulants and antiplatelet drugs, come in various forms. Aspirin and Clopidogrel inhibit platelet function, reducing blood clots. Warfarin and Dabigatran target different parts of the clotting cascade, preventing the formation of fibrin, a protein essential for clot formation.
Interdisciplinary Collaboration: Key to Safe Surgery
Managing blood thinners for dental surgery requires a team effort. Your physician, dentist, and pharmacist work together to assess your risk, develop a tailored plan, and ensure your safety. Open communication among these professionals is vital to minimize complications.
Tailored Blood Thinner Management Strategies
There are several ways to manage blood thinners before and after dental surgery. Your physician may advise you to temporarily stop taking your medication or adjust your dosage. In some cases, they may recommend antifibrinolytic drugs to further reduce bleeding. Additionally, platelet transfusions may be needed to enhance blood clotting.
Patient Education and Informed Consent
Understanding your blood thinner management plan is essential for your well-being. Your healthcare providers will thoroughly educate you on the risks and benefits of each strategy. They’ll also request informed consent, ensuring you fully comprehend the potential outcomes and give your approval for any necessary procedures.
Blood thinner management for dental surgery is a complex but necessary process. By carefully assessing your risks, collaborating with a skilled team of healthcare professionals, and following your instructions diligently, you can ensure a safe and successful dental experience. Remember, patient education and informed consent are key to minimizing complications and promoting a positive outcome.
Blood Thinner Management for Dental Surgery
Entities Involved
Dental Procedures
Dental procedures that typically require blood thinner management include:
-
Tooth extraction: Removing a tooth, which can cause significant bleeding due to the disruption of blood vessels.
-
Dental surgery: This general term encompasses a wide range of procedures that involve cutting and manipulating tissue in the mouth. Bleeding risks vary depending on the complexity and invasiveness of the surgery.
-
Oral surgery: More specialized procedures that often involve extensive tissue removal or manipulation, such as jaw reconstruction, tumor removal, or cleft lip and palate repair. These procedures pose higher bleeding risks.
Blood Thinner Management for Dental Surgery: A Collaborative Effort
Managing blood thinners for dental surgery requires a meticulous collaborative approach involving several healthcare professionals. Each professional plays a pivotal role in ensuring patient safety and optimal outcomes.
The Physician: Prescribing Doctor
The physician is responsible for:
- Assessing the patient’s bleeding and thromboembolic risks
- Prescribing blood thinners and monitoring their effects
- Communicating with the dentist and pharmacist to develop a comprehensive management plan
The Dentist: Performing Surgery
The dentist is responsible for:
- Evaluating the potential bleeding risks associated with the dental procedure
- Coordinating with the physician to adjust blood thinner therapy if necessary
- Monitoring the patient for any signs of bleeding complications
The Pharmacist: Dispensing Medications
The pharmacist is responsible for:
- Dispensing blood thinners and other medications as prescribed
- Providing patient education on medication usage and potential side effects
- Monitoring for drug interactions and ensuring adherence to instructions
The Importance of Collaboration
Effective communication among these professionals is paramount:
- The physician provides medical guidance, assessing the patient’s overall health and adjusting treatment plans as needed.
- The dentist evaluates the procedural risks and collaborates with the physician to modify blood thinner therapy if warranted.
- The pharmacist ensures that medications are dispensed and used correctly, addressing any concerns or questions from the patient.
This interdisciplinary collaboration ensures that patients receiving blood thinners receive tailored dental care that minimizes risks and promotes optimal outcomes.
Blood Thinner Management for Dental Surgery: A Collaborative Effort
The Importance of Interdisciplinary Communication
Blood thinner management for dental surgery is a complex undertaking that requires the expertise of multiple healthcare professionals. Effective collaboration among physicians, dentists, and pharmacists is paramount to ensure the patient’s safety and well-being throughout the process.
Physicians play a crucial role in assessing the patient’s bleeding and thromboembolic risks, and prescribing the appropriate blood thinner management strategies. Dentists, with their specialized knowledge of dental procedures, can identify potential bleeding risks associated with specific interventions and develop a tailored treatment plan. Pharmacists, as experts in medication management, can provide guidance on the proper administration and dosing of blood thinners.
Clear and timely communication among these professionals is essential. Physicians should provide detailed information about the patient’s blood thinner regimen, including any necessary adjustments or discontinuations before dental surgery. Dentists should communicate any potential bleeding risks associated with the planned procedure to the physician and pharmacist. Pharmacists, in turn, should ensure that the patient understands the instructions for their blood thinner regimen and monitor them for any potential interactions or side effects.
By working together, these professionals can create a comprehensive plan that balances the risks and benefits of blood thinner management, ensuring a safe and successful dental surgery outcome.
Blood Thinner Management for Dental Surgery: A Patient’s Guide
If you’re taking blood thinners, the thought of dental surgery can be a bit daunting. But with proper planning and management, you can undergo dental procedures safely.
Understanding Blood Thinners and Dental Risks
Blood thinners, also known as antithrombotics, prevent blood clots from forming. However, they can also increase the risk of bleeding. The type of dental procedure and your medical history determine your bleeding risk.
Similarly, age, medical conditions, and genetic factors influence your risk of developing blood clots. Your doctor will assess both risks to determine the best blood thinner management strategy.
Managing Blood Thinners Before and After Surgery
Your doctor may adjust your blood thinner dosage or prescribe other medications to minimize bleeding during surgery. Platelet transfusions or antifibrinolytic drugs can also be used to control bleeding.
To reduce the risk of blood clots after surgery, your doctor may recommend compression stockings or early ambulation (walking). These measures promote blood flow and prevent clots from forming.
Collaboration and Informed Consent
Communication between your physician, dentist, and pharmacist is crucial. They will work together to develop a personalized plan that balances bleeding and thromboembolic risks.
Informed consent is also essential. Your healthcare providers will discuss the risks and benefits of different management strategies. Understanding your options empowers you to make informed decisions about your care.
Patient Responsibilities
Following instructions and monitoring for complications are vital. Take medications as prescribed, avoid strenuous activity, and watch for signs of bleeding or swelling. Report any concerns to your dentist or physician promptly.
Proper blood thinner management can ensure a safe and successful dental experience. By working closely with healthcare professionals and understanding the risks and benefits involved, you can maintain your oral health while minimizing complications.
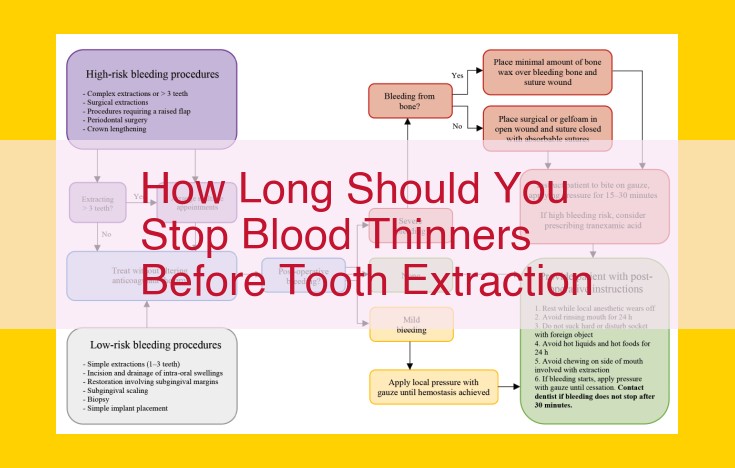
Blood Thinner Management for Dental Surgery: Controlling Bleeding Risks
In the realm of dental care, it’s crucial to manage blood thinners effectively to prevent excessive bleeding during surgeries. One of the most important steps in this management is assessing the bleeding risk associated with the specific dental procedure and the patient’s medical history.
Platelet Transfusions
Platelets are essential blood components that play a vital role in clotting. In certain situations, such as when the patient’s platelet count is critically low, a platelet transfusion may be necessary. This transfusion involves administering platelets from a donor to the patient, effectively increasing their ability to form blood clots and control bleeding.
Antifibrinolytic Drugs
Another valuable tool in controlling bleeding during dental surgery is the use of antifibrinolytic drugs. These medications work by preventing the breakdown of fibrin, a protein involved in the formation of blood clots. By preserving the fibrin network, antifibrinolytic drugs help stabilize the clot and reduce blood loss.
Other Measures
In addition to platelet transfusions and antifibrinolytic drugs, several other measures can be employed to control bleeding during dental surgery, including:
- Topical hemostatic agents: Applied directly to the surgical site, these agents promote clot formation and minimize bleeding.
- Sutures: Skilled suturing techniques can seal incisions and prevent blood from escaping.
- Pressure packs: Applying pressure to the surgical site using gauze or sponges can help compress the blood vessels and reduce bleeding.
- Controlled hypotension: In some cases, inducing a temporary drop in blood pressure can help minimize bleeding during surgery.
By carefully assessing bleeding risks, employing appropriate strategies, and collaborating closely with healthcare professionals, it’s possible to effectively manage blood thinners and ensure safe and successful dental surgeries.
Blood Thinner Management for Dental Surgery: Strategies to Minimize Thromboembolic Risk
Managing blood thinners before and after dental surgery is crucial to prevent excessive bleeding and thromboembolic events like blood clots. Following established guidelines ensures a safe and successful surgical outcome for patients taking anticoagulants or antiplatelet medications.
Understanding the Risk:
Assessing the patient’s bleeding and thromboembolic risk is essential before any dental procedure. Factors like the type of surgery, the patient’s medical history, and genetic predispositions are considered during this assessment.
Strategies to Reduce Thromboembolic Risk:
To prevent blood clots after dental surgery, healthcare professionals may employ various strategies:
-
Compression Stockings: Wearing compression stockings helps promote blood flow in the legs, reducing the risk of deep vein thrombosis (DVT).
-
Early Ambulation: Encouraging patients to move around soon after surgery helps prevent blood from pooling in the veins and forming clots.
-
Anti-Embolism Stockings: Similar to compression stockings, anti-embolism stockings offer additional support to prevent blood clots in the lower extremities.
-
Intermittent Pneumatic Compression Devices: These devices use inflatable cuffs to apply pressure to the legs, mimicking the effects of natural muscle contractions and promoting blood flow.
By implementing these strategies, healthcare professionals aim to minimize the risk of thromboembolic complications during and after dental surgery. These measures complement the use of blood thinners and other interventions, enhancing overall patient safety.
Patient Education and Informed Consent: The Cornerstone of Blood Thinner Management
Patient education plays an indispensable role in ensuring the safety and efficacy of blood thinner management before and after dental surgery. Patients who are adequately informed about their medications, the potential risks, and the importance of following instructions are more likely to participate actively in their care and achieve optimal outcomes. Therefore, healthcare professionals must prioritize patient education to empower them in making informed decisions about their treatment.
During the initial consultation, dentists and physicians should thoroughly discuss the blood thinner management plan with the patient. This discussion should cover the following key points:
- The risks and benefits of different management strategies.
- The potential bleeding and thromboembolic risks associated with dental procedures.
- The importance of following instructions for blood thinner adjustments, such as when to hold or restart medication.
Informed consent is an integral part of patient education. Before any dental procedure, patients should sign a consent form that outlines the risks, benefits, and alternatives to the procedure. By understanding the potential implications of their treatment, patients can make an informed decision about whether to proceed with the surgery and accept the associated risks.
Healthcare professionals should encourage patients to ask questions, voice concerns, and clarify any uncertainties they may have. Empowering patients with knowledge and understanding helps them feel more comfortable and confident in the decision-making process. By fostering open communication and informed consent, patients become active partners in their care, leading to improved adherence, safety, and overall treatment outcomes.
Risks and Benefits of Blood Thinner Management Strategies
When preparing for dental surgery while taking blood thinners, it’s crucial to understand the risks and benefits of the management strategies employed.
Risks
- Bleeding: Blood thinner management can increase the risk of excessive bleeding during and after dental procedures. This is because these medications interfere with the body’s normal clotting mechanisms, potentially leading to prolonged or severe bleeding.
- Thromboembolism: On the other hand, discontinuing blood thinners carries a risk of thromboembolism, a condition where blood clots form in blood vessels. This can occur when the blood becomes too thick and loses its fluidity, leading to potentially life-threatening complications such as strokes, heart attacks, or pulmonary embolisms.
Benefits
Despite these risks, blood thinner management strategies can provide significant benefits:
- Reduced Bleeding: By carefully adjusting or temporarily interrupting blood thinning medication, the risk of excessive bleeding during dental procedures can be minimized. This is particularly important for procedures involving incisions or extractions, where bleeding control is essential.
- Prevention of Thromboembolism: In high-risk patients, continuing blood thinner therapy during dental surgery may be necessary to prevent thromboembolic events, especially when the surgery is complex or prolonged.
Balancing Risks and Benefits
The key to successful blood thinner management in dental surgery lies in balancing these risks and benefits. Healthcare professionals, including physicians, dentists, and pharmacists, collaborate to determine the most appropriate strategy for each patient based on their individual risk factors and the type of dental procedure being performed. This may involve:
- Adjusting Dosages: Modifying the dosage or timing of blood thinners can help optimize bleeding control while minimizing thromboembolic risk.
- Temporary Interruption: In some cases, blood thinners may be briefly interrupted prior to the dental procedure and resumed shortly after, to reduce bleeding risks.
- Additional Measures: Other measures, such as platelet transfusions or the use of antifibrinolytic drugs, may be necessary in certain situations to further control bleeding or prevent clot formation.
Outline the patient’s responsibilities in following instructions and monitoring for complications.
Patient Responsibilities in Managing Blood Thinners for Dental Surgery
As a patient taking blood thinners, your active participation is crucial for a successful dental surgery. Here’s what you need to know:
Follow Instructions
It’s essential to adhere strictly to your doctor’s and dentist’s instructions. They may advise you to adjust your medication dosage or stop taking it altogether before surgery. Do not alter your medication regimen on your own.
Monitor for Complications
After surgery, it’s your responsibility to watch for any signs of bleeding or other complications. Contact your healthcare provider immediately if you experience:
- Excessive or prolonged bleeding from the surgical site
- Bruising or swelling that worsens or doesn’t resolve
- Signs of infection, such as redness, pain, or pus
- Chest pain or shortness of breath (if you’re at risk for blood clots)
Other Responsibilities
- Inform your dental team about all your medications, including blood thinners.
- Follow the post-operative care instructions provided by your healthcare team carefully.
- Avoid strenuous activity for the recommended period after surgery.
- Notify your healthcare providers if you experience any new or worsening symptoms.
Understanding and fulfilling these responsibilities empowers you to proactively manage your health and ensure a smooth dental surgery experience.
Summarize the key points of blood thinner management for dental surgery.
Blood Thinner Management: A Crucial Orchestration for Dental Surgery
Maintaining the delicate balance between bleeding and clotting during dental procedures for patients on blood thinners is a critical aspect of their healthcare journey. Risk assessment is paramount, where doctors and dentists carefully evaluate the patient’s bleeding and thromboembolic risks. This involves considering the type of dental procedure, medical history, and factors like age and comorbidities.
The blood thinners in question can vary in type and mechanism of action. Anticoagulants, like warfarin and heparin, target the clotting process, while antiplatelet drugs, such as aspirin and clopidogrel, prevent platelet aggregation. Understanding these medications and their effects is crucial for effective management.
Dental procedures also pose varying levels of bleeding risk. Tooth extraction, for instance, carries a higher risk than a routine filling. Dentists must be aware of these differences and adjust their approach accordingly.
Healthcare professionals play distinct roles in this management process. Physicians prescribe the blood thinners and assess the patient’s overall health risks. Dentists perform the surgery and monitor bleeding during and after the procedure. Pharmacists dispense the medications and provide patient education. Interdisciplinary communication is vital to ensure seamless coordination and minimize complications.
Blood thinner management strategies vary depending on the patient’s individual risks. Platelet transfusions may be necessary to increase clotting capacity, while antifibrinolytics reduce clot breakdown. Thromboembolic risk reduction measures, such as compression stockings and early mobilization, help prevent blood clots.
Patient education is essential for successful outcomes. Patients must understand the risks and benefits of the management strategies and follow instructions meticulously. They should be aware of signs and symptoms of complications and seek medical attention promptly if needed.
In conclusion, managing blood thinners during dental surgery is a complex but crucial undertaking. Risk assessment, interprofessional collaboration, and patient education are the cornerstones of safe and effective care. By following established guidelines and tailoring strategies to individual patients, healthcare professionals can ensure optimal dental outcomes for those on blood thinners.
Blood Thinner Management for Dental Surgery: Ensuring a Smooth Experience
For patients taking blood thinners, dental surgery can be a source of concern. Managing these medications is crucial to mitigate potential bleeding risks while also ensuring patient safety. Here, we delve into the importance of risk assessment, interdisciplinary collaboration, and patient education to optimize care.
Risk Assessment: A Balancing Act
Before any dental procedure, a thorough risk assessment is essential. This involves evaluating both the bleeding risk associated with the surgery and the thromboembolic risk related to temporarily stopping blood thinners. Factors influencing bleeding risk include the type of procedure and the patient’s medical history, while thromboembolic risk is influenced by age, comorbidities, and genetic factors.
Interdisciplinary Collaboration: A Team Effort
Managing blood thinners for dental surgery is a team effort involving the patient’s physician, dentist, and pharmacist. The physician provides guidance on the best course of action, the dentist assesses the bleeding risk of the procedure, and the pharmacist dispenses and monitors the medications. Clear communication and collaboration among these professionals are vital for safe and effective management.
Patient Education: Empowering Informed Decisions
Informed consent is paramount. Patients should fully understand the risks and benefits of continuing or stopping blood thinners and the strategies employed to manage bleeding. Education empowers patients to actively participate in their care and monitor for any potential complications. By providing clear instructions and encouraging open dialogue, healthcare professionals can foster patient confidence and adherence to the treatment plan.
Risk assessment, interdisciplinary collaboration, and patient education are the cornerstones of safe and effective blood thinner management for dental surgery. By working together, healthcare professionals can minimize bleeding risks, prevent thromboembolic complications, and ensure a positive experience for patients. Patients should be fully informed and actively involved in their care to optimize outcomes and maintain a healthy smile.
Encourage healthcare professionals and patients to follow established guidelines for safe and effective dental care in patients taking blood thinners.
Blood Thinner Management for Dental Surgery: A Guide for Healthcare Professionals and Patients
Imagine you’re getting ready for a dental procedure, and you’re taking blood thinners to prevent dangerous blood clots. You’re understandably concerned about the impact of your medication on your upcoming surgery. Don’t worry; we’re here to help you navigate this process safely and effectively.
Why Blood Thinner Management Matters
Blood thinners are medications that prevent blood clots by reducing your platelet count or interfering with the clotting factors in your blood. While they’re essential for preventing strokes and heart attacks, they can increase your risk of bleeding during dental procedures.
How to Prepare for Dental Surgery
Before your appointment, your healthcare team will discuss your bleeding and clotting risks. They’ll assess your medical history, the type of dental surgery you need, and any other factors that could affect your safety. Communication and collaboration among your physician, dentist, and pharmacist are crucial.
Types of Blood Thinners and Their Effects
- Anticoagulants (like warfarin and heparin) slow down blood clotting by inhibiting clotting factors.
- Antiplatelet drugs (like aspirin and clopidogrel) prevent platelets from sticking together and forming clots.
Blood Thinner Management Strategies
Depending on your individual risks and the dental procedure, your healthcare team may adjust your blood thinner dosage or use additional medications to control bleeding and reduce clotting risk. Strategies can include:
- Platelet transfusions: Replenishing your platelet count to promote clotting.
- Antifibrinolytic drugs: Inhibiting the breakdown of blood clots.
- Compression stockings: Reducing pressure in your legs to prevent swelling and clot formation.
Patient Education and Informed Consent
Informed consent is crucial. Your healthcare team will explain your options, the benefits and risks of each strategy, and your responsibilities in monitoring for complications. Understanding these risks and your role is essential for your safety.
Following Established Guidelines
By following established guidelines, healthcare professionals and patients can ensure safe and effective dental care for individuals taking blood thinners. These guidelines include:
- Risk assessment: Evaluating individual bleeding and clotting risks before surgery.
- Interdisciplinary collaboration: Communication and coordination among the physician, dentist, and pharmacist.
- Patient education: Providing clear information about risks, benefits, and responsibilities.
Remember, dental surgery with blood thinners is manageable with appropriate risk assessment and careful management strategies. By working together with your healthcare team and following established guidelines, you can minimize risks and ensure a successful outcome.