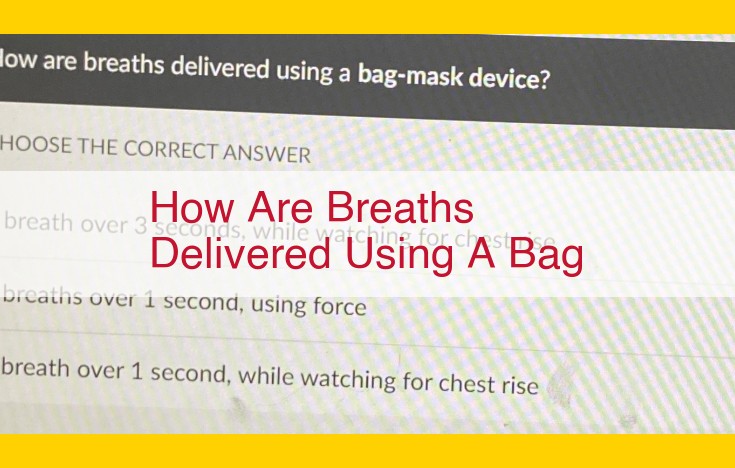
Using a bag-valve mask (BVM), breaths are manually delivered by compressing the bag to force air into the patient’s lungs, creating positive pressure. The BVM consists of a self-inflating bag, a one-way valve, and a facemask that fits over the patient’s mouth and nose, ensuring a proper seal. The healthcare provider places the mask, squeezes the bag, monitors chest expansion, and observes for any signs of resistance or airway obstruction. This technique provides immediate ventilation support in emergency situations or during procedures where spontaneous breathing is inadequate.
Comprehensive Guide to Ventilation: A Breath of Life for Critical Care
- Ventilation, the process of supplying oxygen and removing carbon dioxide from the lungs, forms the cornerstone of patient management in critical care settings.
- It plays a vital role in supporting critically ill patients with impaired respiratory function, enabling them to breathe effectively and maintain adequate gas exchange.
The Importance of Ventilation
- Ventilation ensures optimal tissue oxygenation, which is crucial for vital organ function.
- It helps maintain the body’s acid-base balance by preventing respiratory acidosis (excess carbon dioxide retention) or alkalosis (inadequate carbon dioxide removal).
- Proper ventilation also prevents lung collapse and other pulmonary complications that can arise from inadequate gas exchange.
Comprehensive Guide to Ventilation: Techniques, Equipment, and Monitoring
Ventilation is a crucial aspect of patient management, ensuring adequate oxygen delivery and carbon dioxide removal. It involves healthcare providers,** _respiratory therapists,** and _patients working together to achieve optimal outcomes.
Roles of Healthcare Providers, Respiratory Therapists, and Patients in Ventilation
Healthcare Providers:
- Assess patient’s condition and respiratory needs
- Prescribe ventilation parameters and monitor patient’s progress
- Collaborate with respiratory therapists to provide comprehensive care
Respiratory Therapists:
- Operate and manage ventilation equipment
- Monitor patient’s vital signs and adjust settings accordingly
- Provide respiratory care such as suctioning and chest physiotherapy
Patients:
- Understand their condition and the importance of ventilation
- Cooperate with healthcare providers and respiratory therapists
- Communicate any discomfort or changes in their condition promptly
2. Ventilation Equipment
Bag-Valve-Mask (BVM): A manual ventilation device used for emergencies or when mechanical ventilation cannot be established.
Oxygen Tank or Concentrator: Provides supplemental oxygen to patients with respiratory distress.
Circuitry: Connects the ventilation equipment to the patient’s airway, allowing the flow of gases.
Reservoir Bag: Stores oxygen-rich gas for delivery to the patient during inhalation.
Bag-Valve-Mask (BVM): Your Lifeline in Emergency Ventilation
In the realm of healthcare, the Bag-Valve-Mask (BVM) stands as an indispensable tool for providing life-saving ventilation in emergency situations. This handheld device may seem simple, but its design and functionality are meticulously engineered to restore breathing in critically ill or injured patients.
Description: The BVM comprises three components: a self-inflating bag, a one-way valve, and a mask. The bag’s elasticity allows it to recoil and fill with air when released, generating positive pressure. The one-way valve ensures air flows into the patient’s lungs during inhalation and prevents backflow during exhalation. The mask forms a tight seal over the patient’s mouth and nose, creating an airway for ventilation.
Applications: The BVM’s versatility makes it the go-to device for various scenarios, including:
- Cardiopulmonary resuscitation (CPR): BVM ventilation is essential for maintaining airflow during CPR, assisting the heart in circulating oxygenated blood.
- Surgery and anesthesia: Anesthesia masks are essentially variations of BVMs used to deliver controlled ventilation during surgical procedures.
- Trauma management: BVMs are crucial for providing immediate ventilation to victims of accidents, where maintaining an airway is critical.
Proper Use: Effective ventilation using a BVM requires meticulous technique.
- Position the patient: Ensure the airway is open by tilting the patient’s head back and lifting their chin.
- Apply the mask: Hold the mask firmly over the patient’s mouth and nose, creating a tight seal.
- Squeeze the bag: Compress the bag to generate positive pressure and inflate the patient’s lungs.
- Release the bag: Allow the bag to recoil and refill with air.
- Repeat: Continue rhythmic compression and release of the bag at an appropriate rate to achieve adequate ventilation.
Remember, proper BVM ventilation is a team effort. Clear communication and effective coordination among healthcare providers are essential to ensure efficient and safe operation.
Oxygen Tank or Concentrator: Types, Specifications, and Safety Considerations
In the realm of ventilation, oxygen plays a vital role in sustaining life and supporting recovery. To deliver oxygen effectively, two primary devices are commonly employed: oxygen tanks and oxygen concentrators. Understanding the differences, specifications, and safety considerations associated with each is crucial for optimal patient care.
Oxygen Tanks:
Oxygen tanks are portable, pressurized vessels that store compressed oxygen. Typically made of steel or aluminum, they come in various sizes, ranging from smaller, portable units suitable for emergencies to larger, stationary tanks for extended use. Oxygen tanks provide a reliable and immediate source of oxygen, making them ideal for situations where portability or immediate access is essential.
Oxygen Concentrators:
Unlike oxygen tanks, which contain a finite supply of oxygen, oxygen concentrators generate oxygen from the surrounding air. They typically use a process called pressure swing adsorption to separate oxygen from other gases in the air, providing a continuous flow of oxygen-enriched air. Oxygen concentrators are generally larger and less portable than tanks, but they offer a more cost-effective and environmentally friendly solution for long-term oxygen therapy needs.
Specifications:
When selecting an oxygen tank or concentrator, several key specifications should be considered:
- Flow Rate: This refers to the amount of oxygen delivered per minute, measured in liters per minute (LPM). The flow rate required will vary depending on the patient’s condition and the prescribed oxygen therapy plan.
- Pressure: Oxygen tanks are typically filled to a pressure of 2,000 psi, while concentrators can deliver oxygen at varying pressures. Choosing the appropriate pressure ensures optimal oxygen delivery.
- Purity: The purity of oxygen refers to the percentage of oxygen present in the delivered gas. Medical-grade oxygen typically has a purity of at least 90%.
Safety Considerations:
Oxygen therapy can be life-sustaining, but it also poses potential risks that must be carefully managed.
- Fire Hazard: Oxygen is highly flammable, and contact with heat or sparks can cause explosions. Strict precautions must be taken to prevent smoking, open flames, and electrical devices near oxygen sources.
- Oxygen Toxicity: Prolonged exposure to high oxygen concentrations can lead to oxygen toxicity, which can damage lung tissue and cause other adverse effects. It is crucial to monitor oxygen levels and adjust the flow rate as needed.
- Leaks: Leaks in oxygen tanks or concentrators can result in inaccurate oxygen delivery and pose a safety hazard. Regular inspection and maintenance are essential to prevent leaks.
Circuitry: Composition, Types, and Connection Principles
In the realm of ventilation, circuitry serves as the vital pathway through which gases flow, enabling the exchange of oxygen and carbon dioxide in patients. This complex system comprises multiple components that work in harmony to support respiratory function.
Composition
At the heart of the circuitry lies the ventilator, the driving force that propels gas through the system. From the ventilator, tubing extends, connecting to various components. These include:
- Inspiratory limb: Carries gas from the ventilator to the patient, typically containing a heated humidifier to prevent condensation and reduce airway irritation.
- Expiratory limb: Transports exhaled gas back to the ventilator, often equipped with a bacterial filter to prevent contamination.
- Patient interface: Connects to the patient’s airway, such as a tracheal tube or face mask. It ensures the delivery of gas directly to the lungs.
Types
Circuitry systems vary in their setup, catering to different patient needs. Common types include:
- Single-limb: Typically used for short-term ventilation, featuring a single tube that combines both inspiratory and expiratory functions.
- Double-limb: Employed for long-term ventilation, with separate inspiratory and expiratory limbs to reduce the risk of cross-contamination.
- Closed-circuit: Recirculates exhaled gas, reducing heat and moisture loss from the patient, often used in neonates and patients with lung injury.
Connection Principles
Proper connection of the circuitry is crucial for effective ventilation. The following steps should be followed:
- Ensure correct orientation of inspiratory and expiratory limbs, as indicated by color-coded connectors.
- Tighten all connections securely to prevent gas leaks.
- Check for proper humidifier settings to maintain appropriate temperature and humidity levels in the gas.
- Monitor pressure readings along the circuit to ensure optimal gas flow and avoid potential complications.
- Regularly clean and inspect the circuitry to maintain its integrity and prevent contamination.
By understanding the intricacies of circuitry composition, types, and connection principles, healthcare providers can optimize ventilation outcomes and ensure the well-being of patients during mechanical ventilation.
Reservoir Bag: The Breathing Lifeline
In the realm of ventilation, the reservoir bag is an unsung hero, silently ensuring the flow of life-sustaining breath. This essential component plays a pivotal role in providing optimal ventilation, and its selection and monitoring are crucial for patient well-being.
Function: The Constant Companion
The reservoir bag is the breathing reserve, a flexible pouch that connects to the patient’s airway. It acts as a temporary reservoir of gas, storing the exhaled air and allowing the ventilator to draw it back in during inspiration. This continuous cycle helps maintain a steady supply of oxygen to the patient’s lungs.
Selection: Tailoring to Patient Needs
Choosing the right reservoir bag depends on several factors: patient size, tidal volume, and respiratory rate. Larger bags are suitable for patients requiring higher tidal volumes, such as in mechanical ventilation. Smaller bags are preferred for pediatric patients or those with low respiratory rates, as they reduce the work of breathing.
Monitoring: A Vigilant Watch
Monitoring the reservoir bag is essential to detect any obstructions or leaks that can compromise ventilation. Continuous observation of the bag’s filling and emptying can provide valuable insights into the patient’s respiratory status. Sudden changes in size or shape may indicate a problem, such as a blocked airway or excessive tidal volume. Additionally, the color of the bag can indicate changes in respiratory effort or gas exchange.
By understanding the function, selection, and monitoring of the reservoir bag, healthcare professionals can ensure optimal ventilation for their patients. Together with other ventilation equipment and techniques, this unsung hero plays a vital role in sustaining life and promoting recovery.
Manual Ventilation: Methods, Techniques, and Indications
When a patient’s natural breathing requires assistance, manual ventilation techniques become essential. This crucial intervention, performed by skilled healthcare providers, provides life-sustaining breaths to patients in respiratory distress.
There are various methods of manual ventilation, each with its own unique applications. One common technique is bag-valve-mask (BVM) ventilation. A self-inflating bag is squeezed to deliver breaths through a mask placed over the patient’s nose and mouth. This method is relatively simple and can be used in a wide range of settings, from emergency rooms to ambulances.
Another manual ventilation technique, mouth-to-mask ventilation, involves administering breaths directly from the provider’s mouth to a mask attached to the patient’s airway. This method is more advanced and requires proper training.
The indications for manual ventilation are diverse. It may be used in situations where a patient is apneic (not breathing), has inadequate or shallow breathing, or requires temporary or prolonged respiratory support. Examples include respiratory arrest, cardiopulmonary resuscitation (CPR), and post-operative sedation.
Methods and Techniques
Manual ventilation requires precision and expertise. Here’s an overview of the steps involved:
- Position the patient: Ensure the patient is lying on their back with their airway open and clear.
- Choose the ventilation method: Select the appropriate method based on the patient’s condition and provider’s training.
- Apply the mask: Place the mask snugly over the patient’s nose and mouth, ensuring a seal to prevent air leaks.
- Squeeze the bag: For BVM ventilation, rhythmically squeeze the bag to deliver a breath of approximately 500-1000 mL of volume.
- Control breath rate: Adjust the frequency of breaths based on the patient’s respiratory needs.
- Monitor the patient: Observe the patient’s chest movement, breath sounds, and vital signs to assess the effectiveness of ventilation.
Indications
Manual ventilation is indicated in various circumstances, including:
- Apnea: When a patient is not breathing.
- Inadequate ventilation: When spontaneous breathing is insufficient to meet the patient’s oxygen needs.
- Controlled ventilation: During surgical procedures or when the patient is unable to breathe independently.
- Cardiopulmonary resuscitation (CPR): To provide artificial ventilation during cardiac arrest.
- Temporary support: In cases of respiratory distress or failure while awaiting mechanical ventilation.
Mechanical Ventilation: A Lifeline for Respiratory Support
Intermittent Positive Pressure Ventilation (IPPV)
IPPV is a technique that supports breathing by delivering intermittent breaths of positive pressure to the lungs. This pressure helps open the airways and improve gas exchange. IPPV is commonly used in critically ill patients who require assistance with breathing.
Various settings can be adjusted during IPPV, including tidal volume, respiratory rate, and inspiratory time. The tidal volume is the amount of air delivered with each breath, while the respiratory rate is the frequency of breaths per minute. By fine-tuning these settings, healthcare providers can tailor ventilation to meet the individual needs of each patient.
IPPV is particularly effective in treating hypoventilation, a condition where the body does not receive enough oxygen. It can also be used to manage conditions that prevent spontaneous breathing, such as neuromuscular disorders or drug overdoses.
Positive End-Expiratory Pressure (PEEP)
PEEP is a continuous positive pressure applied to the lungs during expiration. This pressure helps keep the alveoli open, preventing them from collapsing at the end of each breath. PEEP is commonly used to improve oxygenation and reduce airway closure in patients with acute respiratory distress syndrome (ARDS) or other lung injuries.
By maintaining a positive pressure in the lungs, PEEP helps stabilize the alveoli and prevent them from becoming overinflated or collapsed. This improves gas exchange and can reduce the risk of lung damage.
PEEP settings are carefully adjusted by healthcare providers based on the patient’s condition and tolerance. Finding the optimal PEEP level is crucial to achieving the desired benefits without causing side effects such as barotrauma (excessive pressure in the lungs).
Intermittent Positive Pressure Ventilation (IPPV)
In the realm of respiratory support, Intermittent Positive Pressure Ventilation (IPPV) emerges as a cornerstone technique, providing vital breathing aid to critically ill patients. Its essence lies in the intermittent delivery of positive pressure to the lungs, ensuring the optimal delivery of oxygen and removal of carbon dioxide from the bloodstream.
IPPV is commonly employed in patients with acute respiratory failure, where the lungs are unable to maintain adequate gas exchange on their own. It can also be beneficial in those requiring anesthesia or undergoing surgical procedures that impair respiratory function.
The principles of IPPV involve the use of a mechanical ventilator, a sophisticated device that controls the timing, pressure, and volume of delivered breaths. The ventilator is connected to the patient’s airway through an endotracheal tube or a tracheostomy tube.
Settings of IPPV are meticulously adjusted to suit the individual patient’s needs. These settings include:
- Tidal volume: The volume of air delivered with each breath, typically set between 6-8 milliliters per kilogram of ideal body weight.
- Respiratory rate: The number of breaths per minute, adjusted based on the patient’s metabolic demands and respiratory status.
- Positive end-expiratory pressure (PEEP): A level of pressure maintained in the lungs at the end of each exhalation, helping to keep the airways open and improve lung volume.
IPPV offers several indications, including:
- Acute respiratory distress syndrome (ARDS): A severe lung injury characterized by fluid accumulation and impaired gas exchange.
- Pneumonia: An infection that causes inflammation and fluid accumulation in the lungs.
- Chronic obstructive pulmonary disease (COPD): A progressive lung disease that obstructs airflow and makes breathing difficult.
- Neuromuscular disorders: Conditions that weaken or paralyze respiratory muscles, impairing breathing ability.
By providing controlled and tailored respiratory support, IPPV plays a pivotal role in stabilizing critically ill patients, improving their oxygen levels, and promoting recovery from respiratory ailments.
Positive End-Expiratory Pressure (PEEP): Unlocking Respiratory Relief
Navigating the complexities of ventilation can be daunting, but understanding key concepts like Positive End-Expiratory Pressure (PEEP) is crucial for ensuring optimal patient outcomes. PEEP, a cornerstone of mechanical ventilation, is an indispensable tool in the respiratory therapist’s arsenal.
Rationale: Keeping Alveoli Open
PEEP plays a pivotal role in preventing alveolar collapse. When exhalation ends, alveoli tend to shrink due to surface tension. PEEP, by maintaining positive pressure in the airways, counteracts this collapse, keeping alveoli open and enhancing gas exchange.
Applications: Improving Lung Function
PEEP finds its application in various respiratory conditions, including:
- Acute Respiratory Distress Syndrome (ARDS): PEEP improves oxygenation and reduces ventilator-induced lung injury.
- Atelectasis: By preventing alveolar collapse, PEEP helps reinflate collapsed lung areas.
- Pneumonia: PEEP stabilizes alveoli and facilitates surfactant production, aiding in resolving infection.
Monitoring: Striking the Balance
While PEEP offers significant benefits, its optimal level depends on each patient and must be closely monitored. Excessive PEEP can lead to barotrauma, while insufficient PEEP may not provide adequate alveolar recruitment.
Monitoring techniques like capnography and transpulmonary pressure assessment help guide the appropriate PEEP setting. By meticulously balancing these factors, healthcare providers can harness the full therapeutic potential of PEEP.
PEEP, a sophisticated yet indispensable respiratory intervention, has revolutionized the management of acute respiratory conditions. Its ability to keep alveoli open, improve lung function, and prevent complications makes it an invaluable tool in the hands of skilled healthcare professionals.
Tidal Volume: A Crucial Factor in Ventilation
In the realm of ventilation, tidal volume holds a pivotal role. It represents the amount of air that is inhaled and exhaled with each breath, directly impacting the exchange of oxygen and carbon dioxide in the lungs. This vital parameter serves as a cornerstone in determining the effectiveness of ventilation.
To calculate tidal volume, practitioners employ various methods. A common approach involves measuring the volume of air displaced in a spirometer during a single breath. Other techniques, such as esophageal manometry and pneumotachography, provide real-time monitoring of tidal volume during mechanical ventilation.
Optimal tidal volumes vary based on individual patient characteristics, such as age, size, and underlying medical conditions. For healthy adults, 6 to 8 milliliters per kilogram of ideal body weight is often considered appropriate. However, in certain situations, such as acute respiratory distress syndrome (ARDS), lower tidal volumes may be necessary to minimize lung injury.
A well-chosen tidal volume ensures adequate ventilation while avoiding over-inflation of the lungs, a condition known as volutrauma. By maintaining an optimal tidal volume, healthcare providers can strike a balance between meeting the patient’s oxygenation needs and protecting the delicate lung parenchyma from harm.
Respiratory Rate: Determination, Adjustment, and Implications
When providing mechanical ventilation, it is imperative to determine the appropriate respiratory rate for a patient. This vital parameter, often abbreviated as RR, influences several physiological processes and can have significant implications for patient outcomes.
Determining the Respiratory Rate
The respiratory rate is the number of breaths a patient takes per minute. It can be determined by observing chest movements or by using a ventilator, capnography, or other monitoring devices. The typical resting RR for adults ranges from 12 to 20 breaths per minute, but can vary depending on factors like age, activity level, and medical conditions.
Adjusting the Respiratory Rate
The respiratory rate on a ventilator is adjusted based on the patient’s clinical condition, including their oxygenation and ventilation needs. Healthcare providers aim to maintain adequate gas exchange and prevent hypoxemia (low blood oxygen levels) or hypercapnia (high blood carbon dioxide levels).
Implications of Respiratory Rate
Adjusting the respiratory rate can have both positive and negative consequences:
- Increased Respiratory Rate: A higher RR can improve oxygen delivery and gas exchange, but it may also decrease tidal volume and lead to increased airway pressures, which can be harmful to the lungs.
- Decreased Respiratory Rate: A lower RR can reduce airway pressures and the risk of barotrauma (lung injury), but it may also compromise ventilation and lead to elevated carbon dioxide levels.
Monitoring the Respiratory Rate
Continuously monitoring the respiratory rate is crucial to ensure patient safety and optimize ventilation. Healthcare providers use various monitoring techniques, including:
- Capnography: Measures the amount of carbon dioxide in exhaled air, providing insights into ventilation adequacy.
- Pulse Oximetry: Assesses blood oxygen saturation, indicating the effectiveness of gas exchange.
Collaborative Approach
Determining and adjusting the respiratory rate is a collaborative process involving healthcare providers, including respiratory therapists and nurses. Regular monitoring and frequent reevaluation are essential to provide effective ventilation, promote patient comfort, and minimize potential complications.
Oxygen Concentration: Sources, Delivery Methods, and Monitoring
When it comes to ventilation, maintaining adequate oxygen levels is crucial. Oxygen is transported to the patient through various sources and delivery methods, all while carefully monitoring its concentration.
Sources of Oxygen:
- Oxygen Tanks: Portable cylinders filled with pure oxygen. Used in emergencies or for patients requiring a high concentration of oxygen.
- Oxygen Concentrators: Electrical devices that extract oxygen from the ambient air. Provide a continuous supply of oxygen at varying concentrations.
Delivery Methods:
- Nasal Cannula: Thin tubes inserted into the nostrils, delivering oxygen at low concentrations.
- Face Mask: Transparent masks covering the nose and mouth, providing moderate to high concentrations.
- Venturi Mask: Specialized masks that mix oxygen with room air to deliver a precise concentration.
- Tracheostomy Collar: Oxygen is delivered directly into the trachea through a surgical opening, ensuring high concentrations.
Monitoring Oxygen Concentration:
Effective ventilation requires continuous monitoring of oxygen concentration. This is done through:
- Pulse Oximetry: Non-invasive device that measures oxygen saturation in the blood, displayed as a percentage.
- Capnography: Monitors the amount of carbon dioxide exhaled, providing insights into ventilation and oxygenation.
- Blood Gas Analysis: Involves drawing blood to measure oxygen levels directly, offering a precise assessment.
Importance of Oxygen Concentration:
Optimizing oxygen concentration is essential for patient safety. Too high concentrations can lead to oxygen toxicity, while too low concentrations result in hypoxia. By continuously monitoring and adjusting oxygen delivery, healthcare providers ensure adequate oxygenation for optimal patient outcomes.
Capnography: Unveiling the Hidden Breath of Your Patients
As a healthcare professional, you are tasked with ensuring the vitality of your patients. Ventilation plays a crucial role in this mission, allowing us to provide oxygen and remove carbon dioxide from the body. Capnography is an essential tool in this process, shedding light on the hidden depths of a patient’s breath.
What is Capnography?
Capnography is a non-invasive technique that allows us to monitor the concentration of carbon dioxide (CO2) in a patient’s exhaled air, providing a real-time window into their respiratory function. Capnography can be used to monitor patients who are on mechanical ventilation or during procedures such as airway management or sedation.
Applications of Capnography
Capnography has a wide range of applications in clinical settings, including:
- Confirmation of endotracheal tube placement: Ensuring that the airway tube is correctly inserted into the trachea.
- Assessment of ventilation adequacy: Determining if the patient is receiving sufficient ventilation.
- Detection of airway obstruction or disconnection: Identifying issues with the patient’s airway or ventilator circuit.
- Monitoring response to interventions: Assessing the effectiveness of therapeutic interventions, such as bronchodilators or medications.
Interpretation of Capnography
The capnography waveform, which displays the CO2 concentration over time, can provide valuable information about a patient’s respiratory status.
- Normal waveform: A normal capnography waveform has a rapid rise, plateau, and rapid decline.
- Hypoxia: A decreased amplitude of the waveform may indicate hypoxia (low oxygen levels).
- Hypercarbia: An elevated baseline or prolonged plateau may indicate hypercarbia (high carbon dioxide levels).
- Airway obstruction: A delayed rise or decreased waveform amplitude may indicate airway obstruction.
Capnography is a powerful tool that allows healthcare providers to monitor and assess ventilation, providing valuable insights into a patient’s respiratory status. By understanding the principles and applications of capnography, you can effectively use this technique to improve patient care and outcomes.
Comprehensive Guide to Ventilation: Techniques, Equipment, and Monitoring
Other Monitoring Techniques
Beyond capnography, there are several other vital monitoring techniques employed to ensure optimal ventilation:
Pulse Oximetry: This non-invasive method measures oxygen saturation in the blood using a sensor attached to a finger or earlobe. Pulse oximetry provides real-time information about oxygen delivery to tissues, enabling prompt adjustments to ventilation parameters.
Ventilator Alarms: Modern ventilators are equipped with numerous alarms designed to alert healthcare providers to potential problems. These alarms may signal high or low pressures, tidal volumes, or respiratory rates, indicating the need for immediate intervention to prevent patient harm.
End-Tidal Carbon Dioxide (EtCO2) Monitoring: EtCO2 monitoring measures the partial pressure of carbon dioxide in exhaled breath. It provides valuable insights into gas exchange, ventilation adequacy, and metabolic activity. This technique complements capnography but is less invasive and can be used during both spontaneous and mechanical ventilation.
Esophageal Stethoscope: An esophageal stethoscope can be used to auscultate breath sounds through an esophageal balloon. This method is particularly useful in assessing the effectiveness of chest compressions during cardiopulmonary resuscitation (CPR) or in patients with difficult airway management.
Transthoracic Impedance Monitoring: This technique uses electrodes placed on the chest to measure electrical impedance changes associated with chest movement. It allows continuous monitoring of tidal volume, respiratory rate, and patient effort, providing valuable information without the need for invasive procedures or external sensors.
Troubleshooting Common Ventilation Problems
Ventilation can be a lifesaving intervention, but it’s not without its challenges. Healthcare providers encounter various ventilation problems, and identifying and addressing them promptly is crucial for patient safety.
One common problem is inadequate ventilation. This can occur due to factors such as improper mask fit, kinked tubing, or inadequate tidal volume. To troubleshoot this issue, check the mask fit, inspect the tubing, and adjust the ventilator settings as necessary. If the problem persists, consider manual ventilation to ensure adequate oxygenation.
Another issue is patient-ventilator dyssynchrony. This occurs when the patient’s respiratory efforts are not in sync with the ventilator, leading to ineffective ventilation. Troubleshooting this problem involves assessing the patient’s respiratory pattern, adjusting the ventilator settings, and providing relaxation techniques to reduce patient anxiety.
High airway resistance is another potential problem. This can be caused by bronchospasm, excessive secretions, or a narrow airway. To address this, bronchodilators may be administered, secretions suctioned, and the airway may be suctioned. In severe cases, intubation or tracheostomy may be necessary.
If the patient is agitated or fighting the ventilator, it’s important to calm them down and explain the procedure. Sedatives may be necessary in extreme cases. Mechanical problems can also occur, such as leaks in the circuit or equipment malfunctions. Troubleshooting these issues requires thorough inspection and prompt replacement or repair of faulty components.
By systematically troubleshooting ventilation problems and working collaboratively with the patient, healthcare providers can ensure effective ventilation, optimize patient outcomes, and minimize complications.
Considerations for Special Patient Populations
When it comes to ventilation, special considerations must be taken for certain patient populations. These include:
Infants:
Infants have immature lungs and a higher respiratory rate. They also have a smaller tidal volume and require specialized ventilation devices. Mechanical ventilation is often used for infants with respiratory distress syndrome or other conditions that impair breathing.
Obese Patients:
Obese patients have a higher risk of developing respiratory complications during ventilation. They have a decreased lung compliance and increased airway resistance. Positive end-expiratory pressure (PEEP) may be used to improve lung compliance and reduce the risk of atelectasis.
Trauma Victims:
Trauma victims often have multiple injuries that can affect their ventilation. They may have chest wounds, lung contusions, or other injuries that impair breathing. Mechanical ventilation is often used to stabilize the patient’s condition and improve oxygenation.
Additional Considerations
In addition to the special considerations for these patient populations, other factors must be taken into account when providing ventilation. These include:
- Patient positioning: The patient’s position can affect lung expansion and ventilation.
- Medications: Some medications can impair respiratory function and should be used cautiously in ventilated patients.
- Nutritional support: Adequate nutrition is essential for maintaining respiratory function. Ventilated patients may require enteral or parenteral nutrition.
Ventilation is a complex and critical procedure that requires careful consideration of the patient’s individual needs. By understanding the special considerations for different patient populations and following best practices, healthcare providers can provide optimal ventilation support and improve patient outcomes.
Comprehensive Guide to Ventilation: Techniques, Equipment, and Monitoring
Unveiling the crucial world of ventilation, a life-sustaining therapy essential in patient management. It’s a collaborative journey involving healthcare providers, respiratory therapists, and patients, each bearing a vital role.
Ventilation Equipment
Embark on an exploration of the tools that make ventilation possible:
- Bag-Valve-Mask (BVM): A manual device for emergencies, delivering oxygen via a mask.
- Oxygen Sources: Cylinders or concentrators provide life-giving oxygen.
- Circuitry: Tubes connecting components, ensuring efficient gas flow.
- Reservoir Bag: Compensates for changes in patient’s breathing, maintaining pressure.
Ventilation Techniques
Discover the different ways to provide ventilation:
- Manual Ventilation: A hands-on approach, utilizing the BVM to manually inflate the lungs.
- Mechanical Ventilation: Machines assist breathing, with IPPV delivering intermittent pressure and PEEP maintaining airway patency.
Ventilation Parameters
Understanding the critical parameters that guide ventilation:
- Tidal Volume: The volume of air delivered per breath.
- Respiratory Rate: The number of breaths per minute.
- Oxygen Concentration: The percentage of oxygen in the gas mixture.
Monitoring
Ensuring patient well-being during ventilation:
- Capnography: Measuring carbon dioxide levels to assess lung function.
- Other Monitoring Methods: Pulse oximetry, ventilator alarms, and more.
Troubleshooting and Special Considerations
Navigating the challenges of ventilation:
- Common Ventilation Problems: Identifying and resolving issues like leaks or airway blockages.
- Special Patient Populations: Understanding ventilation needs for infants, obese patients, and trauma victims.
Ventilation is an intricate interplay of techniques, equipment, and monitoring. Its success lies in the collaboration of healthcare providers and the active participation of patients. By comprehending the key aspects of ventilation management, we empower ourselves to optimize patient outcomes and provide the best possible care.
Emphasize the Importance of a Collaborative Approach Among Healthcare Providers
In the intricate world of patient care, effective ventilation management demands a symphony of expertise that reverberates throughout the healthcare team. It’s not merely a solo performance but a collaborative masterpiece where each note, each breath, harmonizes to sustain life and nurture healing.
Physicians conduct the orchestra, providing the blueprint for ventilation based on the patient’s unique needs. Their keen eyes scrutinize vital signs, monitoring the ebb and flow of oxygen and carbon dioxide, guiding the team’s every move.
Respiratory therapists, like virtuoso musicians, command the machinery, adjusting dials and settings with deft precision. Their mastery of ventilation techniques ensures that every breath is delivered seamlessly, nurturing the delicate balance of the patient’s respiratory system.
Nurses, the heartbeat of patient care, become the constant companions at the bedside. Observing diligently, they detect subtle changes in the patient’s condition, ensuring timely adjustments and providing unwavering support and comfort.
This collaborative tapestry extends beyond the hospital walls. Family members and caregivers play a vital role as the unsung heroes, providing emotional buoyancy and practical assistance. Their presence can ease the patient’s anxiety and bolster their spirit, fostering a positive healing environment.
By embracing this collaborative spirit, healthcare providers not only optimize ventilation management but also nurture a sense of trust and partnership with patients and their loved ones. This unyielding commitment to teamwork elevates the quality of care, fostering optimal outcomes and restoring the breath of life to those who entrust themselves to our care.
The Patient’s Role in Effective Ventilation
In the realm of patient care, ventilation plays a crucial role in ensuring proper oxygenation and carbon dioxide removal. While healthcare providers and respiratory therapists are indispensable, the patient’s active participation is paramount in achieving optimal outcomes.
Partnering with the Patient
Effective ventilation requires a cohesive partnership between the healthcare team and the patient. Communication is key, as the patient’s feedback regarding their comfort and any unusual sensations provides valuable insights for adjusting ventilation parameters.
Self-Monitoring
Patients can monitor their respiratory rate and oxygen saturation using portable devices such as pulse oximeters. By recording these readings and sharing them with their healthcare providers, patients contribute to a personalized and responsive ventilation plan.
Active Participation in Treatment
Patients can actively participate in their ventilation by performing controlled breathing exercises. This includes following instructions on how to coordinate breaths with the ventilator and practicing deep breathing to prevent atelectasis.
Education and Empowerment
Educating patients about the purpose and settings of their ventilator empowers them to take an active role in their care. This understanding helps to dispel anxiety and foster a sense of control.
Empowered Patients, Improved Outcomes
By involving patients in the ventilation process, healthcare providers can improve patient comfort, compliance, and overall outcomes. Empowered patients are more likely to engage in self-monitoring, actively participate in their treatment, and experience a smoother recovery.